What Happens If I Need a Pacemaker But I Have An Allergy?
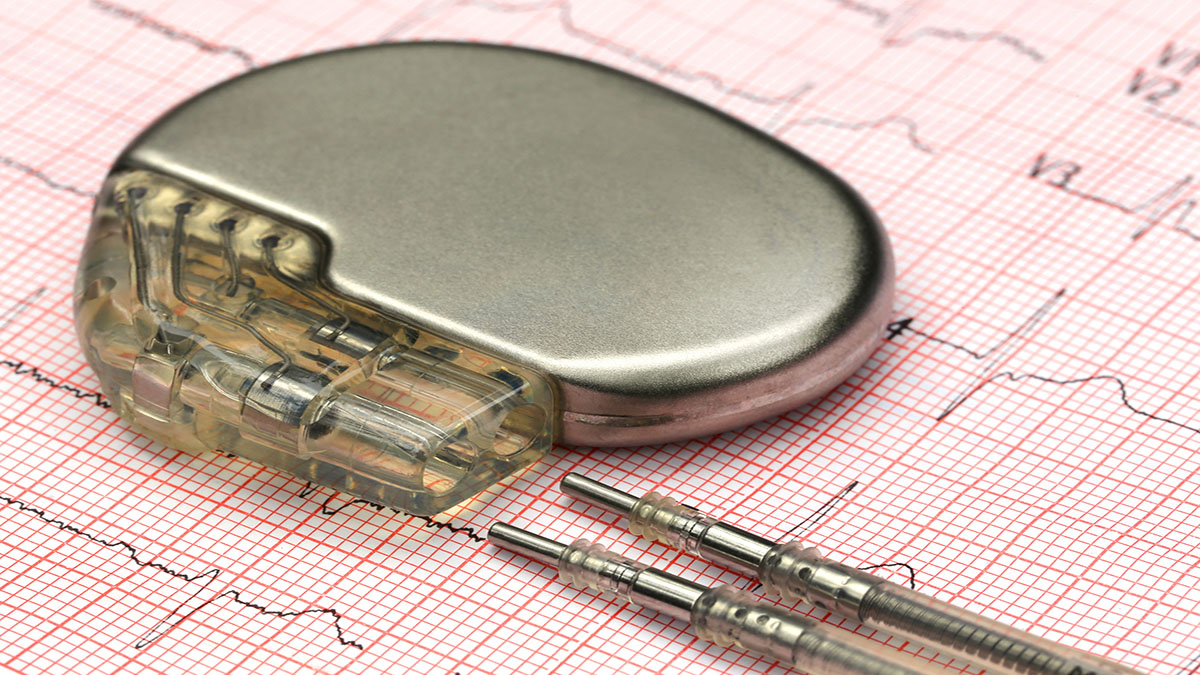
A pacemaker is a device put inside the body to help support the electrical system of the heart. Sometimes, allergic reactions can happen because of a compound in the device. Drs. Tom Callahan and Bruce Wilkoff from electrophysiology talk to Dr. John Anthony, Dermatology and Dr. James Taylor, Clinical Professor of Dermatology about what to do if someone has an allergy but needs a lifesaving device.
Learn more about the Cardiac Electrophysiology and Pacing Section at Cleveland Clinic
Subscribe: Apple Podcasts | Buzzsprout | Spotify
What Happens If I Need a Pacemaker But I Have An Allergy?
Podcast Transcript
Announcer:
Welcome to Love Your Heart, brought to you by Cleveland Clinic's Sydell and Arnold Miller Family Heart, Vascular and Thoracic Institute. These podcasts will help you learn more about your heart, thoracic and vascular systems, ways to stay healthy, and information about diseases and treatment options. Enjoy.
Thomas Callahan, MD:
Hello, and welcome to the podcast. Today we're talking about allergies, and specifically allergies to cardiac implantable devices. This is brought to you by Cleveland Clinic and LEADConnection.org. I'm Tom Callahan. We're joined by Dr. Bruce Wilkoff, who's director of the Lead Extraction Center at Cleveland Clinic and founder of LEADConnection, Dr. Jim Taylor, who is a clinical professor of dermatology at the Cleveland Clinic Lerner College of Medicine, and Dr. John Anthony, section head of occupational and contact dermatology at Cleveland Clinic. Welcome to you all.
Bruce Wilkoff, MD:
Thank you.
James Taylor, MD:
Yes, thanks.
Thomas Callahan, MD:
Dr. Wilkoff, you've been implanting devices for a long time, so you've seen a lot of things. How common are these allergic reactions to our devices?
Bruce Wilkoff, MD:
Well, fortunately, quite rare. But the problem is that it's suspicioned or suspected much more commonly, and the much more common problem is an infection or a hematoma, we haven't talked about that too much, but hematomas, infections are much more likely things, than even a superficial infection. We must consider it every time a patient comes with a problem with their incision in their pocket, pain or whatever. It's rare, but it does happen, and when we do that, we need to work together, teamwork is important here.
Thomas Callahan, MD:
Agreed. Dr. Anthony, can you talk about who's perhaps at highest risk for these types of allergic actions to medical devices? What sort of things should patients be thinking about and talking to their doctors about before surgery, before an implant like this.
John Anthony, MD:
I think it is important for patients to be complete and work with their team early on to identify potential concerns. Because the devices are made of multiple components, we would want people who have had problems with metals in the past to talk with their doctor about that, whether it's a piercing or jewelry or a snap on clothing, those can be relevant. History of sensitivities and metals.
We would want people to talk about problems with antibiotics, topical antibiotics, for example. Those things that you can purchase over the counter that contain polymyxin B or neomycin or bacitracin, all very common, but sometimes can cause allergies.
Also, for example, patients who have problems with glues or acrylates specifically like acrylic nails or gel nails, shellac nails, those kinds of acrylic sensitivities that lead to rashes on the fingers would also be really useful. Of course, if you have intolerance to bandages or electrode leads, please tell your doctors that before you have a procedure done.
Thomas Callahan, MD:
That's great advice. Dr. Taylor, what types of testing do we do? I know that this can be a challenging diagnosis to make, but what sort of testing is available for patients where there's a concern for this type of allergy?
James Taylor, MD:
Well, the testing that we most commonly perform is called patch testing, which is a procedure for diagnosing the types of reactions that Dr. Anthony was reporting and describing. Patch test is for delayed hypersensitivity, so it's in contrast to going to your allergist that you may have seen for, say, asthma or allergic rhinitis or hay fever, where they prick the skin and read it immediately.
The patch testing involves applying the different metals and other components to your skin. They're left on for two days or 48 hours, removed, and the site evaluated, and then the patient returns in another, usually 48 hours, to have further evaluation of the site. The patch testing for allergic contact dermatitis is generally considered the gold standard to make the diagnosis.
There are blood tests that have been used in some cases. We generally don't rely on those. Occasionally in conflicting results with patch testing, we may do that, but generally patch testing is the gold standard that we use, along with the history Dr. Anthony outlined, and the location and the clinical appearance of the rash.
Thomas Callahan, MD:
That's great. Thank you. Dr. Wilkoff, if a patient has a device like a pacemaker or a defibrillator, and they're concerned they might have some sort of allergic reaction to the device, what should they do? What advice do you give to those patients?
Bruce Wilkoff, MD:
What I say to every patient, and it's not your job to figure out what the problem is. It's your job to bring it up to our attention so we can work it out. Nine times out of 10, it's nothing, and I can reassure you and worrying doesn't help, so asking is the thing to do. The thing that we have today that we haven't had before is the ability to take pictures and send them to our doctors, and the pictures are very useful. Now, pictures are not the same thing as examining you, but it does help. Ask the question, bring it up, send a picture, and then we'll take it from there.
Thomas Callahan, MD:
Excellent. Dr. Anthony, can you talk a little bit about treatment for these allergic reactions to implantable devices?
John Anthony, MD:
Thank you. Because this is a very relatively rare thing, there aren't specific treatment guidelines that exist, so treatment has to be the decision of your team approach. There should be multiple people involved in this, and it can be dermatology, it can be allergy, it can be obviously your cardiology team, infectious disease. It's important to have lots of people involved for complicated problems, and so that team should come together to help create a treatment plan specific and personalized for that patient.
Thomas Callahan, MD:
That's excellent. Well, I want to thank everyone very much for joining the conversation. Until next time.
John Anthony, MD:
Thanks, Tom.
Bruce Wilkoff, MD:
Thanks, Tom.
Announcer:
Thank you for listening. We hope you enjoyed the podcast. We welcome your comments and feedback. Please contact us at heart@ccf.org. Like what you heard? Subscribe wherever you get your podcasts or listen at clevelandclinic.org/loveyourheartpodcast.

Love Your Heart
A Cleveland Clinic podcast to help you learn more about heart and vascular disease and conditions affecting your chest. We explore prevention, diagnostic tests, medical and surgical treatments, new innovations and more.


