Recurrent Pericarditis New treatment shows promise
Patients with pericarditis may be on various medications to prevent episodes from recurring. Dr. Allan Klein, Director of Cleveland Clinic’s Pericardial Disease Center, provides the results of the RHAPSODY trial that looked at a new medication (Rilonacept) vs. placebo for patients with pericarditis. He talks about the exciting results of this study and what this may mean for patients in the future.
Read the article on Consult QD
TranscriptAnnouncer:
Welcome to Love Your Heart, brought to you by Cleveland Clinic's Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute. These podcasts will help you learn more about your heart, thoracic and vascular systems, ways to stay healthy, and information about diseases and treatment options. Enjoy.
Dr. Allan Klein:
My name is Dr. Allan Klein from the Cleveland Clinic. I'm the Director of the Center for the Diagnosis and Treatment of Pericardial Diseases. It's my great pleasure to present the results of RHAPSODY. This is the pivotal Phase 3 trial of rilonacept in patients with recurrent pericarditis. I'd like to acknowledge my co-principal investigator from Italy, Dr. Massimo Imazio, as well as all of the other authors, the investigator, the site staff, and of course, all the patients that were involved with the study.
Dr. Allan Klein:
For those patients out there with recurrent pericarditis, let me fill you on what this is all about. Recurrent pericarditis is a chronic debilitating auto inflammatory disease, often requiring months to years of treatment. There's no FDA-approved therapies at the current time. Nonspecific immunosuppressants are commonly used, such as NSAIDs, ibuprofen, colchicine, and corticosteroids. But corticosteroids are associated with significant morbidity.
Dr. Allan Klein:
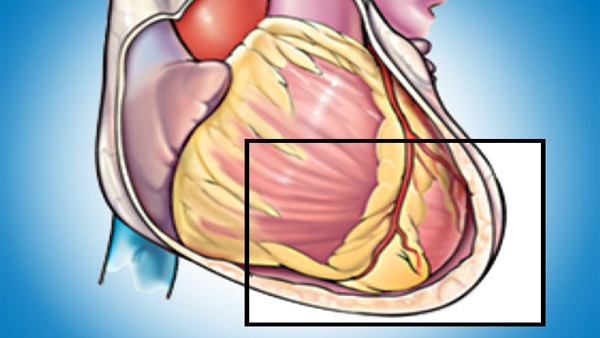
Interleukin-1 has been implicated as a key mediator of recurrent pericarditis and rilonacept, as shown over here, is a once-weekly IL-1 alpha and IL-1 beta cytokine trap. I've shown in the diagram here ... Let me tell you how this works. So for example, if you get a viral illness and you damage the pericardial cell, what happens is the pericardial cell releases IL-1 alpha. This attracts macrophages, which is like white cells, and the macrophages activate what you call the inflammasome. The inflammasome secretes IL-1 beta, and the IL-1 alpha and beta attach to the capillaries, the blood vessels, and cause capillary leak and inflammation. If you had a drug that targets IL-1 alpha and beta, this may help patients suffering from recurrent pericarditis.
Dr. Allan Klein:
Let me tell you about the RHAPSODY trial. The RHAPSODY trial was designed to test the hypothesis that monotherapy, single drug with rilonacept will be sufficient to resolve active episodes of recurrent pericarditis and also reduce the risk of a pericarditis recurrence. The trial was unique because it utilized a randomized withdrawal design. Acutely symptomatic patients like you out there that are failing their background regimen of end-stage colchicine or steroids, were enrolled in a 12-week single blind run-in period, which they received rilonacept while other pericardium medications were tapered and discontinued, including the steroids and colchicine and NSAIDs. Those patients that responded to the monotherapy rilonacept were then randomized one-to-one to either continue the rilonacept or placebo in a double-blind event-driven randomized withdrawal period.
Dr. Allan Klein:
What we looked at as a primary efficacy endpoint was basically the time to first adjudicated pericarditis recurrence. Those patients who experienced recurrence of pericarditis could be given open label bailout rilonacept, remain in the study. Also, we looked at major secondary efficacy endpoints related to patient symptomatology. I should point out that there's a long-term extension period to the study, which is ongoing up to 24 months where patients can get open label rilonacept.
Dr. Allan Klein:
Who are those patients that were enrolled in the RHAPSODY trial? These are patients that are very common to you in the community. It was a very well-balanced study. There was 57% female, 43% male, mainly Caucasian. The average age was 44.7 years. The number of pericarditis episodes prior to enrollment was 4.7. As you could see, patients were experiencing acute recurrence despite 80% treated with colchicine, and almost half that were on steroids. These patients were experiencing very serious disease because the Pericarditis Pain Score, out of 10 was 6.2, and their C-reactive protein was over six milligrams per deciliter. As well, 38% had pericardial fusion, 50% had a pericardial rub, and 19% had EKG changes. Who were enrolled in this study? Of 86 patients enrolled, 79 patients completed the run-in. Of those, 61 patients were eventually randomized in the randomized withdrawal period. The long-term extension period is ongoing for some of these patients.
Dr. Allan Klein:
Now, the results. As you can see in this slide, rilonacept initiation resulted in a very rapid resolution of the acute episode. During the run-in period, we saw a rapid and sustained reduction in both the pain shown in the purple bar and gray, inflammation to CRP as soon as after the first dose of rilonacept. The median time to get the pain response was five days, and the median time for the CRP to normalize was seven days.
Dr. Allan Klein:
Importantly, all patients who were receiving steroids at baseline successfully tapered off and were transitioned to single drug or monotherapy rilonacept within eight weeks. In terms of the primary efficacy endpoint, the study met this, as shown here. In total, there was a total of 25 events. Only two in the rilonacept arm and 23 in the placebo arm. The median time to first adjudicated pericarditis recurrence in placebo patients was 8.6 weeks after randomization. Almost half of those who went on to suffer recurrence did so within the first month. In contrast, in rilonacept arm, the median time to recurrence couldn't be calculated since there was not enough events. Statistically, the hazard ratio was 0.4 with a highly statistically significant P-value of less than 0.0001.
Dr. Allan Klein:
This corresponds to a very dramatic 96% reduction in the risk of a recurrent pericarditis event. Of note, there were no reported recurrences for the remainder of the randomized withdrawal period in patients receiving bailout rilonacept. The annualized incidence of recurrence on treatment was reduced compared to pre-study. That was the primary efficacy endpoint.
Dr. Allan Klein:
Now the secondary endpoints. All three major secondary efficacy endpoints at week 16 were highly statistically significant. Of note, four times as many rilonacept patients maintained a clinical response compared to placebo. From a patient quality of life perspective, 81% of patients receiving rilonacept reported absent or minimal pericardial symptoms compared to 25% of placebo recipients. Finally, rilonacept recipients reported 98% of trial days being pain-free or at most experiencing minimal chest pain versus 46% of placebo recipients. All these endpoints, the sensitivity analysis were consistent out to week 24 with curve separation as early as week eight.
Dr. Allan Klein:
So you may be asking, "Was this drug safe?" Well, rilonacept was generally well tolerated. The events were consistent with the known safety profile of rilonacept. Of note, there were no drug-related serious adverse events and importantly, no deaths. Non-serious adverse events in four patients led to discontinuation, all during the run-in period and not during the randomized withdrawal period. The most common side effect or events were injection site reactions and upper respiratory tract infections.
Dr. Allan Klein:
In conclusion, in the RHAPSODY trial for patients like you in the audience with symptomatic recurrent pericarditis on end-stage colchicine and prednisone, and you're failing the standard of care therapy, these data demonstrate a very robust and dramatic treatment response to rilonacept, including resolution of acute episode, reduced risk of recurrence by 96%, a corticosteroid-sparing effect and finally, improved quality of life.
Dr. Allan Klein:
So in terms of the perspective, how we treat patients with recurrent pericarditis in 2020, this study, the RHAPSODY trial, could now represent a paradigm shift in how we treat patients in that rilonacept not only provided a steroid-sparing effect to half the study population that were on steroids, but in the future may obviate the need for steroids and go right to rilonacept despite having a recurrence with colchicine.
Dr. Allan Klein:
Many of you out there may be asking, "Is rilonacept currently available?" Well, first of all, it is already approved as a drug called Arcalyst in rheumatology for the CAP Syndrome. But for recurrent pericarditis, it's undergoing regulatory review by the FDA and is considered breakthrough therapy. So we hope that within the year that this drug will be approved. I should also mention that the results of the RHAPSODY trial will be published in the New England Journal of Medicine. Thank you very much for your attention.
Announcer:
Thank you for listening. We hope you enjoyed the podcast. We welcome your comments and feedback. Please contact us at heart@ccf.org. Like what you heard? Subscribe wherever you get your podcasts or listen at clevelandclinic.org/loveyourheartpodcast.
Subscribe: Apple Podcasts | Buzzsprout | Spotify
Recurrent Pericarditis New treatment shows promise

Love Your Heart
A Cleveland Clinic podcast to help you learn more about heart and vascular disease and conditions affecting your chest. We explore prevention, diagnostic tests, medical and surgical treatments, new innovations and more.


