A PFO closure uses a medical device to close an opening between your heart’s two upper chambers. You only need this opening as a fetus. After birth, when your lungs are working, this opening usually closes. When it stays open, it usually doesn’t cause issues. But in some cases, it does. PFO closure is an option for people whose PFOs cause problems.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
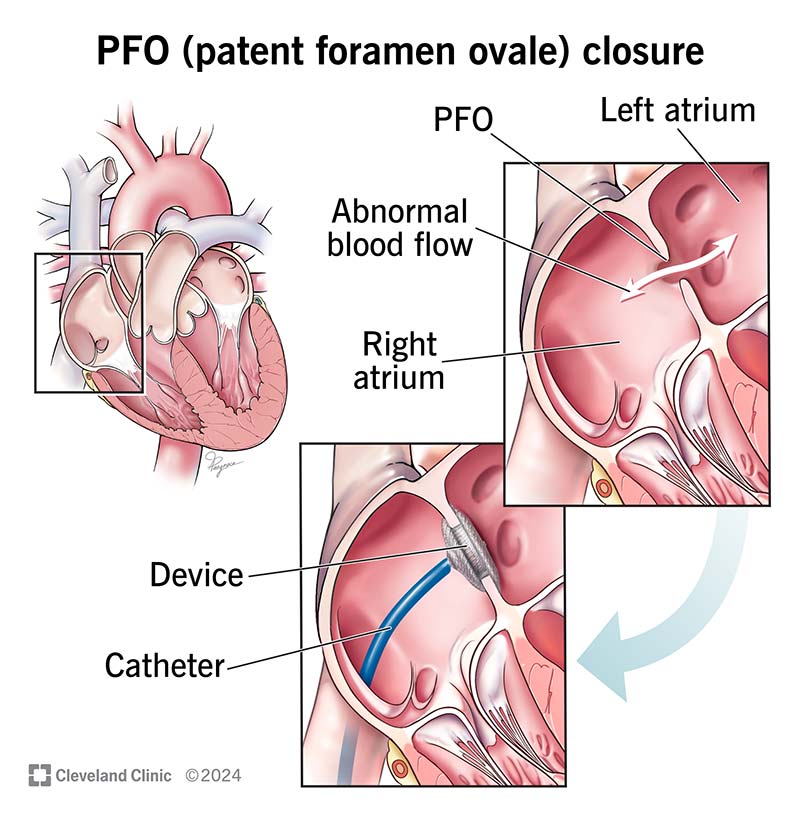
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17326-patent-foramen-ovale)
A PFO (patent foramen ovale) closure plugs an opening between your heart’s two upper chambers by putting in a permanent device. A healthcare provider can do this using a catheter (a long, thin, flexible, hollow tube) that they get to your heart through a large vein elsewhere in your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your provider can use a closure device to plug the opening. These devices have a wire frame that consists of a nickel-titanium metal alloy with synthetic material around it. Some look like a yo-yo, with two round disks and a narrow middle. Each round disk covers one side of the hole in your heart.
Within a few days of receiving a PFO closure device, your body’s own tissue will start to grow over and around it. Three to six months later, your heart tissue completely covers the device. At that point, it becomes a part of your heart wall.
If you have a PFO larger than 25 millimeters, a provider will probably do PFO closure surgery instead of using the catheter method. This is rare.
A PFO closure plugs an opening (a foramen ovale) in your heart that usually closes at birth. As a fetus, you need a PFO (patent foramen ovale) to allow blood to flow from your right atrium (upper heart chamber) to your left atrium. But you don’t need it after birth because your lungs are breathing oxygen instead of taking it from your birth mother's blood.
The PFO closure device will stay in your heart permanently to stop the abnormal flow of blood between the two atrial (top) chambers of your heart.
When should a PFO be closed?
Advertisement
A healthcare provider may recommend a PFO closure procedure if:
It’s not common for people to need a PFO closure. About 25% of people have a PFO, but most people don’t need treatment for it.
You’ll need to get several tests before your procedure, like:
To prevent blood clots, you’ll also need to start taking medicines like aspirin and clopidogrel before your PFO closure. Your provider will tell you when to start taking these. During your procedure, your provider will also give you heparin to prevent blood clots.
During a PFO closure, a provider will:
The cardiac catheterization procedure for a PFO closure typically takes one to two hours.
Within 24 hours after the procedure, a provider will do tests to make sure your PFO closure device is in the right place. Tests include:
Before you leave, your provider will prescribe medications for you to take at home. You’ll need to take aspirin or other blood-thinning drugs like clopidogrel every day for six months or longer to prevent blood clots from forming.
You’ll need to take antibiotics one hour before certain medical procedures (like dental cleaning, dental surgeries and other surgeries) for up to six months after you receive the device. Your provider will tell you which procedures will require antibiotic pre-treatment to prevent endocarditis. They may tell you to delay a dental procedure for six months instead.
Like all medications, take them only as directed. Never stop taking the medication without talking with your provider first. And call your provider if you have any unpleasant reactions to, or concerns about, the medicine.
Benefits of PFO closure include:
Advertisement
A study found a success rate of about 96% for implanting a PFO closure device in hundreds of people without serious complications.
Risks or complications of PFO closure may include:
Healthcare providers don’t consider a PFO closure a risky procedure. This is especially true when an experienced provider performs it. Still, about 7% of people with a PFO closure have complications. They’re more likely to happen if you’re older than 60.
You’ll need to rest in bed in the hospital for six hours after patent foramen ovale closure. You may go home the evening of the procedure or the following morning.
After you go home:
Advertisement
You’ll need a few follow-up visits over the next year to monitor your heart and the device’s placement. These appointments will be one month, six months and one year after your procedure. Each visit will include a chest X-ray, electrocardiogram and echocardiogram.
Some researchers say a PFO closure doesn’t reduce your stroke risk much more than medication.
But others have found that having a catheter-based procedure for PFO closure and taking blood-thinning drugs like aspirin gives people a lower rate of stroke than people who received only aspirin. People who had a PFO closure had a risk of stroke at least 45% lower than people who took the medicine but didn’t have a procedure.
Contact your provider if you have signs of the complications in the list above. This may include bleeding or signs of infection in the area where they put the catheter.
This is a question without a simple answer. Everyone’s situation is different. Talk with your healthcare provider about your case to decide if a PFO closure is right for you. You can discuss the benefits and disadvantages of PFO closure.
Airport or other security sensors, household appliances or medical imaging methods won’t affect your PFO closure device. But the wire frame on the device may reduce the clarity of magnetic resonance imaging (MRI) or computed tomography (CT) images slightly. For this reason, be sure to tell the imaging technician that you have this device in your heart.
Advertisement
You’ll receive an identification card that you should carry with you to show to medical personnel, if necessary.
Deciding on a PFO closure can be a difficult decision. The best thing you can do is have an honest conversation with your healthcare provider about your specific case. Ask about the pros and cons of treating a PFO with medicine or with a procedure. Learn what you can about PFOs and don’t be afraid to ask questions if anything isn’t clear.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic Children’s cardiology providers are experts in diagnosing and treating the congenital heart condition, patent foramen ovale (PFO).
