Goodpasture syndrome is a potentially life-threatening autoimmune disorder. It causes your immune system to attack tissues in your lungs and kidneys. Symptoms include trouble breathing and coughing up blood. Without treatment, it can lead to lung damage, kidney failure and death. Treatment includes medications and a type of blood transfusion.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
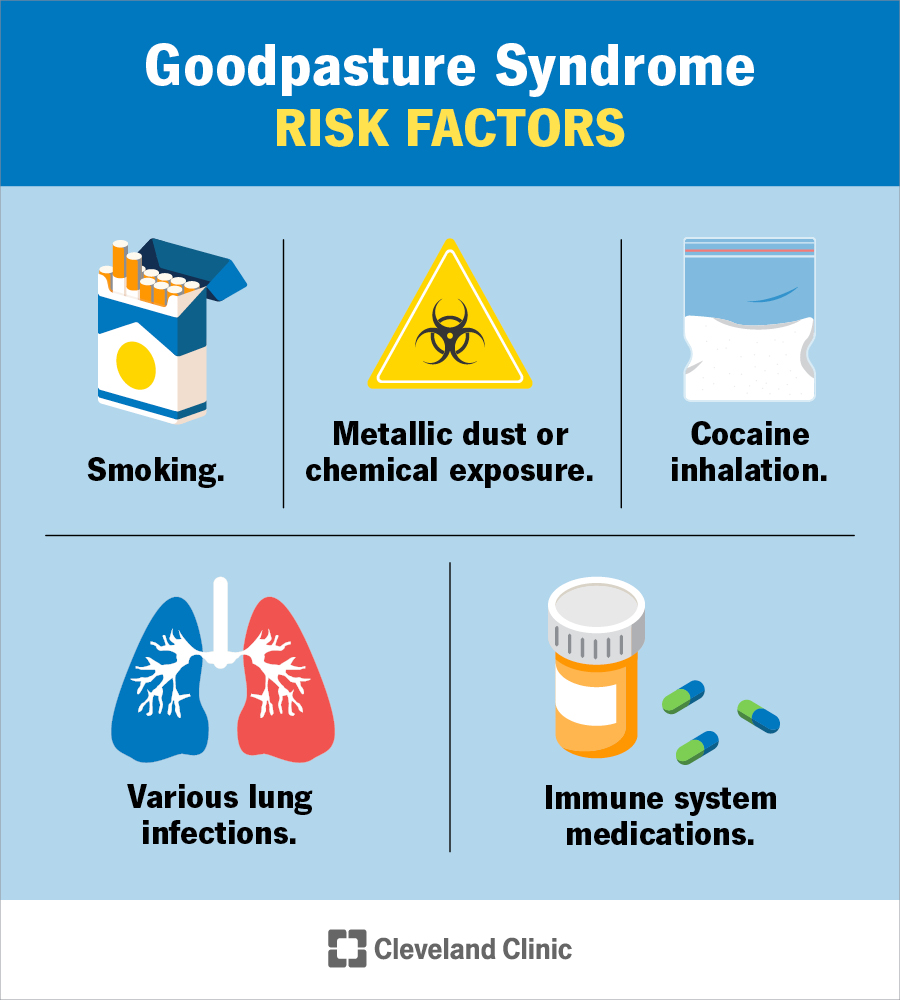
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/5927-goodpasture-syndrome)
Goodpasture syndrome is a rare, life-threatening autoimmune disease that affects your kidneys and lungs. It happens when your immune system attacks collagen because it mistakes it as foreign. Collagen is a protein that helps make up your:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If you have Goodpasture syndrome, your body produces proteins (antibodies) that attach to collagen in certain parts of your lungs and kidneys. When this happens, it causes inflammation and destroys the tissues. Without treatment, Goodpasture syndrome can cause kidney inflammation (glomerulonephritis) that can lead to kidney failure. It can also cause severe bleeding in your lungs (pulmonary hemorrhage), which is the main cause of death from Goodpasture syndrome.
Other names for Goodpasture syndrome include:
Goodpasture syndrome is very rare. Healthcare experts report fewer than two new cases per 1 million people yearly.
Goodpasture syndrome is a pulmonary-renal condition. That means it affects your lungs (pulmonary) and kidneys (renal). Lung-related symptoms usually appear first. They include:
Kidney-related symptoms include:
Advertisement
Goodpasture syndrome causes your immune system’s antibodies to attack collagen in the glomerular basement membrane (GBM) of your kidneys. The GBM is part of your glomeruli. Glomeruli are tiny blood vessels in your kidneys that help filter your blood. Anti-GBM antibodies also attack collagen in your lungs’ air sacs. This destroys lung tissue, which leads to bleeding and difficulty breathing.
Healthcare providers and medical researchers aren’t exactly sure what causes your immune system to overreact to collagen. It may result from a combination of environmental factors and the genes you inherit from your biological parents. Studies of people with Goodpasture syndrome have shown a strong association with human leukocyte antigen (HLA) DR15. HLAs are proteins that help your immune system tell the difference between your tissues and invading substances.
Sometimes, Goodpasture syndrome can develop after an infection, like a cold or the flu. You may also be more likely to develop it if you:
Goodpasture syndrome affects people of all ages. But it more often affects those early in life (teens to 30s), then again in the 60s and 70s.
A healthcare provider will ask about your symptoms and perform a physical exam. They’ll also order tests to help diagnose Goodpasture syndrome, including:
Yes, with proper diagnosis, Goodpasture syndrome is treatable.
Goodpasture syndrome treatment can vary depending on its severity. Healthcare providers treat mild cases with medications, including:
Advertisement
Providers also use plasmapheresis. During this procedure, they use a needle to remove blood from a vein in your body, usually your arm. They separate the liquid part of your blood (plasma) from the blood cells. The plasma contains the harmful anti-GBM antibodies. They replace your plasma with healthy plasma from blood donors and return it to your body.
You may need to take immunosuppressant drugs for six to 12 months. In most cases, you need plasmapheresis every day for several weeks.
Without treatment, Goodpasture syndrome may cause life-threatening bleeding in your lungs. It can also lead to kidney failure. But with an early diagnosis, treatments are effective. Your immune system will only make the antibodies for a short period — a few weeks up to two years. Relapses or recurrences of the disease are very rare.
The most severe complication of Goodpasture syndrome is kidney failure. Kidney failure treatment requires dialysis or a kidney transplant.
The five-year survival rate for people with Goodpasture syndrome is 80%.
You may not be able to prevent Goodpasture syndrome. But you can lower your risk by avoiding:
Advertisement
If you have Goodpasture syndrome, it’s a good idea to:
See a healthcare provider right away if you’re coughing up blood, having trouble breathing, peeing less than usual or having any other symptoms of Goodpasture syndrome. Early diagnosis can significantly improve your outlook. Without treatment, Goodpasture syndrome can cause permanent kidney damage or fatal lung problems.
In medicine, a triad is a group of three symptoms that describe a medical condition. The triad of Goodpasture syndrome is:
It can be frustrating and isolating to have Goodpasture syndrome, especially because healthcare providers don’t yet know what causes it. It can interrupt your daily life and even force you to change jobs if you work around metal dust, gasoline, tar or asphalt.
Advertisement
Talking to a healthcare provider as soon as you notice symptoms is crucial. Early diagnosis and treatment reduce your chances of developing life-threatening bleeding in your lungs or long-term damage to your kidneys.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Goodpasture syndrome is a rare autoimmune disease that affects your lungs and kidneys. At Cleveland Clinic, we know what to look for and what treatments work.
