Pseudogout is arthritis that causes sudden flares of pain, swelling and stiffness in your joints. It’s called pseudogout because it causes similar symptoms that come and go just like gout. But it’s a different condition. Gout happens when there’s too much uric acid in your blood. A buildup of calcium pyrophosphate dihydrate (CPP) causes pseudogout.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
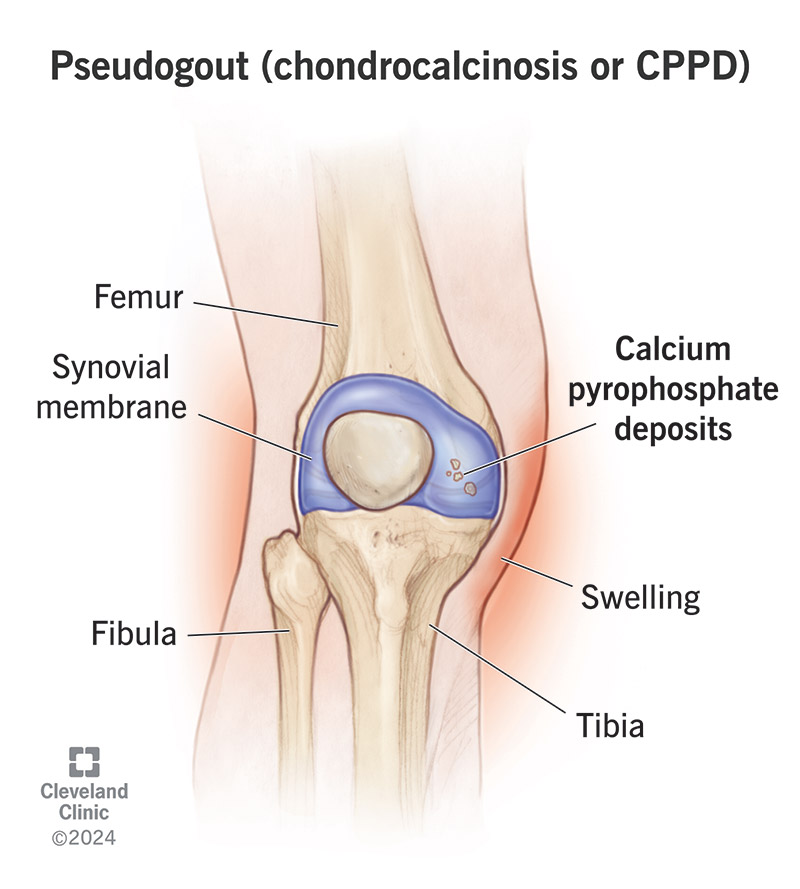
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/pseudogout-chondro-calcinosis-cppd)
Pseudogout is a form of arthritis that causes sudden episodes of pain and swelling in your joints.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Pseudogout can affect any joint in your body, but it’s most common in:
Healthcare providers also call pseudogout other names, including:
All of these names refer to the same condition.
Pseudogout gets its name from how similar it is to gout, another type of arthritis that causes the same kinds of symptoms. “Pseudo” is a prefix that means false, so pseudogout is “false” gout.
Gout happens when there’s too much uric acid in your blood (hyperuricemia) and sharp uric acid crystals clump together in your joints and cause inflammation.
A buildup of a different crystal in your joints causes pseudogout — calcium pyrophosphate (CPP). That’s why calcium pyrophosphate deposition is another name for pseudogout. Deposition means something being deposited.
Gout most commonly affects the joint where your big toe connects to the rest of your foot (the metatarsophalangeal, or MTP joint). Pseudogout doesn’t usually develop in the MTP joint, and is much more common in other, bigger joints.
The most common pseudogout symptoms include:
Advertisement
Pseudogout symptoms come and go (recur) in episodes called flares or attacks. Pseudogout attacks can happen suddenly. You’ll usually notice symptoms all at once, rather than feeling them slowly building up over time. A flare of pseudogout symptoms can last anywhere from a few days to a few weeks (or longer).
A buildup of calcium pyrophosphate (CPP) in your affected joints causes pseudogout. The extra CPP forms small crystals that build up in the cartilage and fluid-filled synovial membranes cushioning your joints. Eventually, the CPP crystals clump together inside your joints and cause a flare of pseudogout symptoms.
Experts aren’t sure what causes your body to make extra CPP. Some studies have found that it might be hereditary, meaning that parents can pass the risk of developing pseudogout to their biological children. Some people develop it after experiencing trauma or an injury that damages a joint. Experts think certain metabolic or endocrine conditions can cause pseudogout.
Anyone can develop pseudogout, but it’s much more common among people older than 65. Having certain health conditions can increase your pseudogout risk, including:
People with other types of arthritis may be more likely to develop pseudogout, too, including:
People with untreated pseudogout also have more frequent and severe flares. Some people with pseudogout experience headaches or neck pain. This can happen if the CPP deposits form around the dense bone in your upper neck.
A healthcare provider will diagnose pseudogout with a physical exam and some tests. Your provider will examine your joints and ask about the symptoms you’re experiencing. Tell your provider:
Your provider may do a joint aspiration (arthrocentesis) to confirm that you have extra CPP crystals in your joint fluid. They’ll insert a needle into your joint, withdraw some fluid and send the sample to a lab. A lab technician will look at the sample of your joint fluid using a microscope. Finding excess CPP crystals in your joint fluid after an aspiration is usually the best way to confirm pseudogout.
A joint aspiration can hurt, especially if you’re experiencing severe symptoms in that joint. Your provider can give you numbing medication so you feel less pain during the aspiration.
Advertisement
Your provider may also use imaging tests to look for chondrocalcinosis (signs of CPP buildup). Your provider might take pictures of your joints and the tissue around them with:
Your provider will suggest treatments to manage the symptoms you’re experiencing and reduce how often you have pseudogout attacks. The most common treatments are medications, including:
Advertisement
You should expect to have flares of symptoms that come and go. Flares can happen more frequently if you don’t get pseudogout diagnosed and treated by a healthcare provider.
Even if you’re treating pseudogout, people usually experience flares more often as they age.
For now, there’s no way to prevent pseudogout. But experts are researching what exactly makes your body produce the extra CPP that causes it.
Managing any other health conditions you have can reduce how often you experience symptom flares.
Some people naturally experience symptoms more often than others. It’s not your fault, and you didn’t do something wrong or unhealthy if you experience a pseudogout attack. It doesn’t usually have direct causes (triggers) you can modify or avoid.
Visit a healthcare provider if you experience sudden, intense pain in any of your joints, especially if your joint is also swollen and your skin is red or discolored. Pseudogout shares many symptoms with gout, infections and other issues that need treatment right away.
Talk to your provider if you’re having more frequent pseudogout attacks or if your symptoms are more severe than they used to be.
Questions to ask your provider include:
Advertisement
What you eat or drink doesn’t usually trigger pseudogout attacks. But it can trigger gout attacks. That’s one of the major differences between pseudogout and gout.
Eating certain foods or drinking alcohol can trigger gout flares. Your body can produce extra uric acid when it breaks down foods or drinks high in chemicals called purines. That’s why following a low purine diet is a common way to manage gout.
Your provider might suggest that you eat or avoid certain foods to maintain your overall health or manage other conditions you may have. But calcium pyrophosphate crystals don’t build up in your body the same way uric acid can, so pseudogout isn’t usually connected to what you eat or drink.
Pseudogout might mean “false” gout, but there’s nothing fake about the pain, swelling and discomfort you’re feeling. It’s frustrating to learn that you can’t prevent pseudogout. But most people are able to find a combination of medications that minimizes how much (and how often) pseudogout affects their daily routines.
You’ll still probably experience flares periodically, but your provider will help you find ways to manage symptoms.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic experts can diagnose gout so you can begin treatment to relieve pain. We help alleviate symptoms and prevent future gout flares.
