Hyperparathyroidism is when your parathyroid glands produce too much parathyroid hormone (PTH). This can cause high levels of calcium in your blood. Hyperparathyroidism can be primary (caused by growths or enlarged glands) or secondary (caused by kidney disease or low calcium levels). Treatments include surgery, medications and lifestyle changes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hyperparathyroidism is a condition where one or more of your parathyroid glands is overactive and releases (secretes) too much parathyroid hormone (PTH). This can cause hypercalcemia, or high levels of calcium in your blood.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You have two pairs of parathyroid glands (four total) in your neck. Their job is to make sure you have enough calcium in your blood. They also reduce blood phosphate levels. They secrete PTH to send signals to:
Your kidneys then send active vitamin D to your gut, which tells it to absorb calcium. Vitamin D also sends a signal back to your parathyroid glands, telling them when your body has enough calcium and they should stop releasing PTH.
When your parathyroid glands make more than enough PTH, your bones can lose too much calcium, making them thin and brittle. The calcium can also build up in your kidneys, blood vessels, heart and other parts of your body.
Types of hyperparathyroidism include:
Advertisement
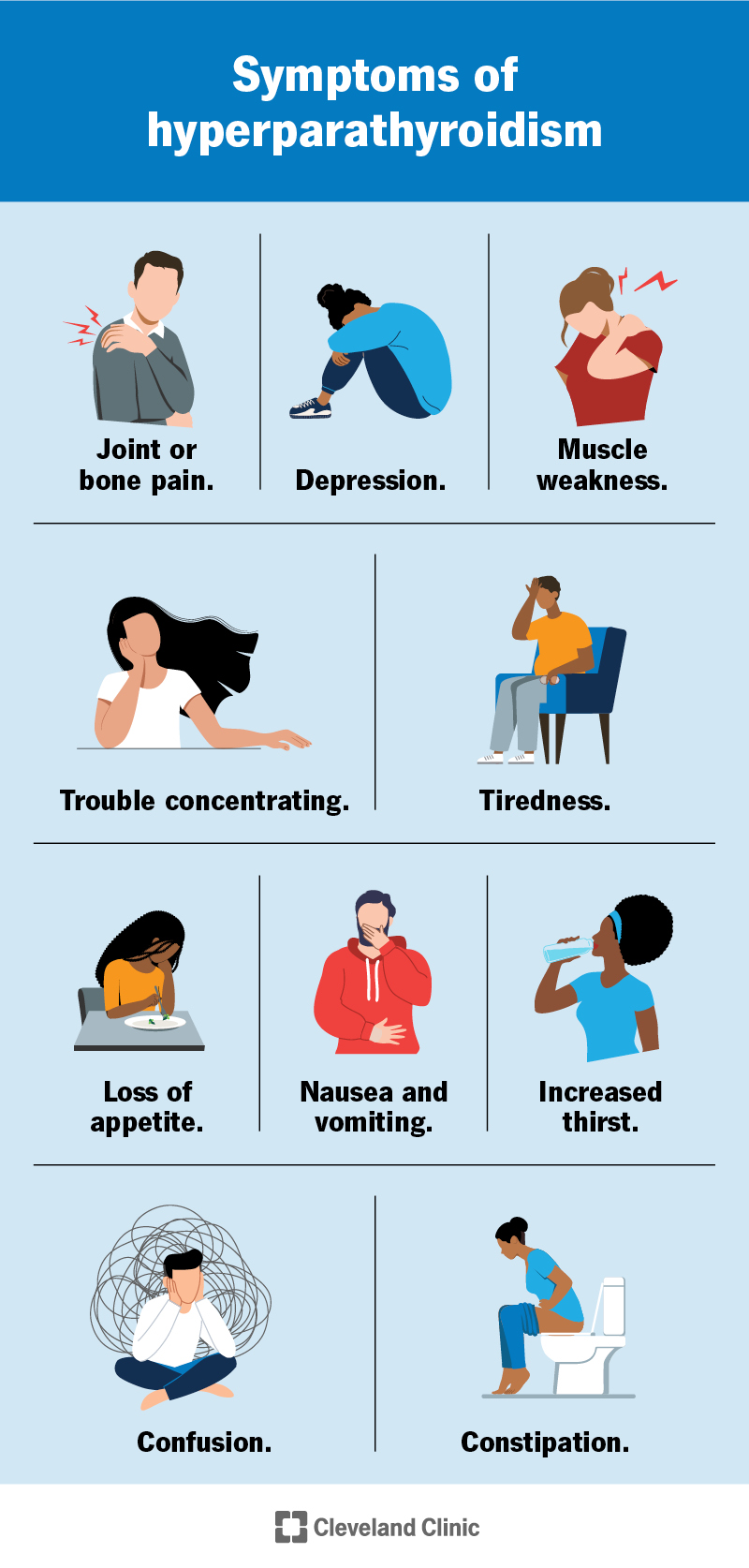
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/14454-hyperparathyroidism)
Symptoms of hyperparathyroidism, especially in people with high calcium levels, include:
Sometimes you don’t have symptoms of hyperparathyroidism. Instead, you’re diagnosed during a routine blood test or tests for other conditions.
Growths on your parathyroid glands, parathyroid gland enlargement, and conditions that cause low levels of calcium or high levels of phosphate can all cause hyperparathyroidism. Primary, secondary and tertiary hyperparathyroidism have different causes.
When you have a growth on a parathyroid gland or one or more of the glands are enlarged, it produces more PTH and doesn’t respond to signals that tell it to stop making hormones. This causes primary hyperparathyroidism. Specific causes of primary hyperparathyroidism include:
The most common cause of secondary hyperparathyroidism is kidney disease. When your kidneys aren’t working properly, your phosphate levels go up and your vitamin D levels go down. Low vitamin D levels lead to low calcium levels. Your parathyroid glands adjust by making more PTH to get rid of phosphate in your blood and increase the amount of calcium. Your body can usually keep up a balancing act for a while, but eventually, it won’t be able to keep up, and hypercalcemia can start damaging parts of your body.
Low vitamin D levels — from lack of sun or malnutrition — can also sometimes cause secondary hyperparathyroidism.
Secondary hyperparathyroidism causes tertiary hyperparathyroidism. Your parathyroid glands become enlarged from working much more than they should. This causes them to stop responding to signals that tell them not to make more PTH.
Certain factors can put you at a higher risk for hyperparathyroidism. They include:
High levels of calcium in your blood can cause additional health conditions, including:
Advertisement
Healthcare providers diagnose hyperparathyroidism by measuring your calcium, vitamin D and parathyroid hormone levels. They’ll also check your kidney function.
Primary hyperparathyroidism causes high levels of calcium in your blood and pee, and low levels of phosphate in your blood. Secondary hyperparathyroidism causes low levels of vitamin D, normal or low levels of calcium and high levels of phosphate in your blood. Providers often find hyperparathyroidism during routine tests before you have symptoms.
Tests providers use to diagnose and monitor hyperparathyroidism include:
Advertisement
The type of treatment depends on whether you have primary or secondary hyperparathyroidism. Treatments could include surgery, supplements and/or lifestyle changes.
Surgery to remove a growth or an enlarged parathyroid gland (parathyroidectomy) can cure hyperparathyroidism. Your provider might be more likely to recommend surgery if you’re younger than 50 or you have:
If you don’t have surgery, your provider will monitor your symptoms, calcium levels and kidney function. They may also recommend or prescribe:
Advertisement
Treating secondary hyperparathyroidism can be complex. You and your provider will work together to treat the root cause. If you have chronic kidney disease, you might need dialysis or a kidney transplant. Your provider may recommend talking to a dietitian about a kidney-friendly meal plan, like avoiding phosphorus, and/or prescribe medications. Medications may include:
If these strategies don’t work or if you develop tertiary hyperparathyroidism, your provider will probably recommend surgery.
If you have hyperparathyroidism and don’t have surgery, you’ll need to monitor your symptoms. You might also need to make changes to what you eat or take medications or supplements. Once or twice per year, your provider will test your:
For people with primary hyperparathyroidism, parathyroidectomy is very effective at bringing calcium levels back to normal, and at improving bone density and symptoms. Studies suggest that, after surgery, over 80% of people (4 out of 5) saw symptom improvement, and over 90% (9 out of 10) had calcium levels return to normal and bone density improve.
Kidney transplant improves secondary hyperparathyroidism in about 40% of people within a year.
Many people live with primary hyperparathyroidism for years without it affecting their health. But eventually, you may need surgery to treat it. Studies suggest that, of people who don’t have symptoms of primary hyperparathyroidism at the time of their diagnosis, about 25% (1 out of 4) will eventually need surgery.
Managing underlying conditions, like chronic kidney disease, can reduce your risk of secondary hyperparathyroidism. There aren’t specific ways to reduce your risk of primary hyperparathyroidism.
If you have hyperparathyroidism, the following tips can help you take care of yourself:
For some people with hyperparathyroidism and low vitamin D levels, it might make sense to take vitamin D supplements. Always ask your provider what kinds of foods, beverages and supplements you should be looking for — and what you should avoid.
See a healthcare provider if you have symptoms of hyperparathyroidism. If you have another health condition that puts you at risk for hyperparathyroidism, talk to your provider about symptoms to look out for and when you should check in with them.
It might be helpful to ask your healthcare provider:
Some people can manage hyperparathyroidism without it ever affecting their health. For others, especially people with kidney disease, hyperparathyroidism can cause serious complications.
Your parathyroid has good intentions — its job is to give your body the calcium it needs to function. But when it overreacts, it can start harming your body. Parathyroid surgery can cure hyperparathyroidism, and many people can manage hyperparathyroidism without surgery and may never develop symptoms.
But if you have kidney disease that’s causing hyperparathyroidism, you may need to try many different treatments to find something that works for you. Eventually, you may need a kidney transplant or parathyroidectomy. Be sure to talk to your provider about your options, and tell them any symptoms you have. They can help guide you to the best treatment plan for your specific situation.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic treats all parathyroid diseases, including cancer, and their side effects. We’ll create a personalized treatment plan that meets your needs.
