Post-thrombotic syndrome is a group of signs and symptoms that develop as a complication of deep vein thrombosis (DVT). It occurs within two years of your DVT diagnosis in the same affected limb (leg or arm). You may notice pain, heaviness, itching, swelling or redness in your limb. Treatment includes compression therapy and lifestyle changes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Post-thrombotic (postphlebitic) syndrome is a condition that occurs as a complication of deep vein thrombosis (DVT). DVT is the formation of a blood clot in one of the deep veins in your leg or arm. Even with successful DVT treatment, the blood clot can cause lasting damage to your veins. This damage prevents your veins from working as well as they should.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As a result, blood pools in your veins. This pooling of blood raises the pressure in your veins and causes symptoms like pain and swelling. Post-thrombotic syndrome is the medical term for the range of symptoms this vein damage can cause. Some people experience mild symptoms, while others have severe symptoms that greatly affect their daily life.
If you’ve had DVT in the past two years and have symptoms of post-thrombotic syndrome, see a healthcare provider right away. They’ll evaluate your condition and recommend appropriate treatment to help you feel better.
Post-thrombotic syndrome is common among people who’ve had DVT. It affects 20% to 50% of people within two years of their DVT diagnosis.
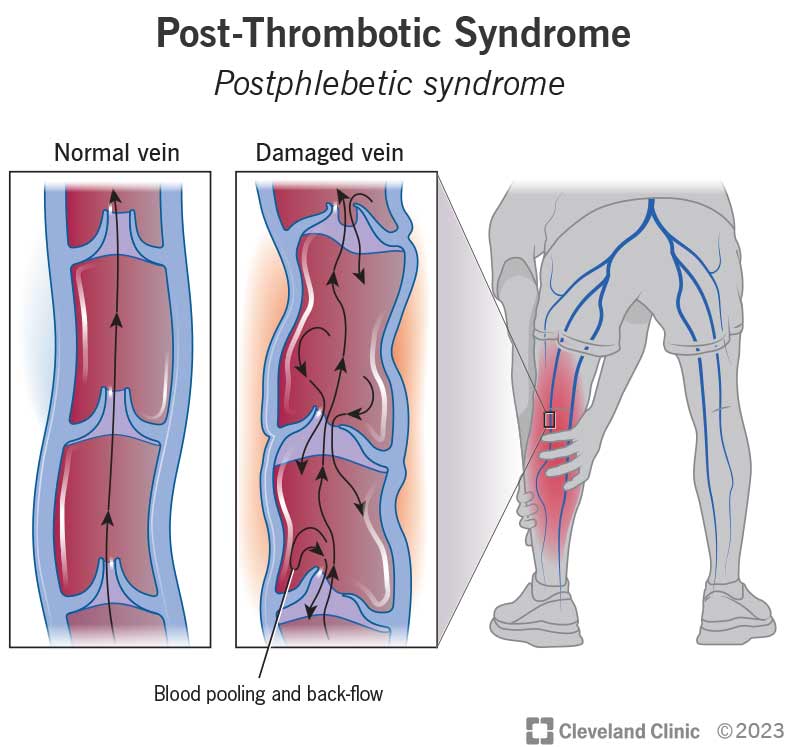
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24936-post-thrombotic-syndrome-illustration.ashx)
If you have post-thrombotic syndrome, blood in your damaged vein has a hard time making it back to your heart. Pooling of blood in your vein can cause pain and other symptoms.
Post-thrombotic syndrome symptoms occur in the limb (leg or arm) where the DVT happened. Symptoms that you may feel in your affected limb include:
Symptoms can range from mild to severe. You may notice your symptoms get worse when you’re walking or standing for a long time and ease when you rest. Symptoms may also feel worse later in the day. You may notice symptoms constantly, or they may come and go.
Advertisement
Signs are things you can see when looking at your leg or arm. Your provider will also look for these signs during an appointment. The signs of post-thrombotic syndrome include:
Deep vein thrombosis (DVT) damages your veins. This damage can cause post-thrombotic syndrome.
The deep veins in your legs and arms contain one-way valves. These valves help keep blood flowing back toward your heart. But the formation of blood clots in your vein can cause lasting damage to those valves, preventing them from working as they should.
As a result, your blood flow grows sluggish. Instead of moving efficiently toward your heart, blood pools in your veins. This raises the pressure inside your vein walls and leads to symptoms.
Anyone who’s had DVT is at risk for post-thrombotic syndrome. However, you face a higher risk if you’ve had recurrent DVT, especially in the same limb. This means you had more than one episode of DVT affecting the same leg or arm.
You may also face a higher risk if the blood clot you had in the past:
Additional risk factors include:
Healthcare providers diagnose this condition with a physical exam. During the exam, your provider will:
Based on this information, your provider will determine if you have post-thrombotic syndrome. They’ll also assess its severity.
You may hear your provider mention the Villalta scale. This is a standard numeric scale providers commonly use to diagnose this condition. You can think of it as a checklist with points attached. It includes five symptoms and six signs. For each symptom and sign, your provider assigns a point value:
Your provider then adds up the points to reach a diagnosis. A total of less than four points means you don’t have post-thrombotic syndrome. A total of five or higher means you do.
Providers further break down the scoring to determine if you have a mild, moderate or severe form of the condition:
Advertisement
Your provider will share the findings with you and discuss what they mean.
There’s no specific diagnostic test for post-thrombotic syndrome. However, in some cases, providers order duplex ultrasound testing to check blood flow through your veins.
Treatment commonly includes compression therapy, lifestyle changes and exercise. Some people need surgical procedures or venous ulcer care. Healthcare providers tailor treatment to each person’s individual needs. The goals of treatment include easing your symptoms and improving your health-related quality of life.
Your provider may recommend you wear compression stockings. These are a common form of compression therapy that can ease your symptoms. You wear the stockings regularly (often daily) according to your provider’s instructions. The stockings squeeze your calf muscles to improve blood flow in your veins. They should feel snug but not painful.
There are different types of stockings that provide varying amounts of pressure. Your provider will prescribe the proper stockings for you based on your needs.
You may need time to adjust to wearing compression stockings. It’s important to talk to your provider about how they feel and whether you’re able to wear them as prescribed. Your provider may adjust the level of pressure as you go along based on how you’re feeling and whether the stockings provide enough symptom relief.
Advertisement
Other forms of compression therapy your provider may recommend include:
Lifestyle changes can play a big role in improving your symptoms. Your provider may recommend you take these actions:
Exercise may help improve blood flow and relieve your symptoms. For example, if post-thrombotic syndrome affects your leg, your provider may recommend exercises that strengthen your leg muscles.
That’s because your calf muscles act as a powerful pump that healthcare providers call a “second heart.” When you walk, the squeezing action of your calf muscles helps blood return to your heart from your legs and feet. So, strengthening those muscles can give your veins the help they need to keep blood moving.
Exercise can also improve your flexibility and cardiovascular endurance. Be sure to talk to your provider before starting a new exercise routine. They’ll make sure you’re doing exercises that are safe and helpful for your needs.
Advertisement
In select cases, providers recommend surgery or an endovascular procedure (like stenting) to improve blood flow in your veins. Your provider will tell you if such treatment options are suitable for you.
Severe cases of post-thrombotic syndrome can lead to venous ulcers. Careful, diligent treatment is essential to avoid serious complications like amputation. Your provider will recommend one or more of the following:
Post-thrombotic syndrome is a chronic condition. That means your healthcare provider can help you manage it, but there’s no cure. Treatments can help ease your symptoms and improve your ability to work, socialize or do other things you enjoy.
You can’t always prevent post-thrombotic syndrome. That’s because it’s not always possible to prevent deep vein thrombosis (DVT). However, you and your provider can work together to lower your risk by:
Your provider will offer guidance for how to care for yourself at home. Follow it closely and ask questions if anything is unclear. General tips include:
It’s also important to pay attention to your mental health. Living with post-thrombotic syndrome can take a toll on how you feel mentally and emotionally. People with this condition often experience depression, anxiety and a general loss of self-confidence. You may worry about blood clots returning. You may miss some of the activities you used to do, which are now more difficult because of your symptoms.
If this sounds familiar to you, it may help to speak with a counselor or therapist. They can help you work through these emotions and find solutions to help you feel better.
Your provider will schedule follow-ups to monitor your condition. It’s essential to go to all of these appointments so your provider can adjust your treatment plan as needed.
Call your provider any time you have new or changing symptoms.
Some questions that may help you learn more about your diagnosis include:
A diagnosis of post-thrombotic syndrome can bring many questions and concerns to your mind. Be assured that your healthcare provider is there to answer your questions and guide you through treatment. This condition is common, but your needs and concerns are still unique. Work with your provider to get resources to support your physical and mental health.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Vascular disease may affect your life in big and small ways. Cleveland Clinic’s specialists treat the many types of vascular disease so you can focus on living.
