A vasospasm is a tightening of an artery that lasts longer than a normal constriction. Vasospasms can happen in many parts of your body, but the most concerning are in your heart and brain. When your blood vessel is narrow, it reduces the amount of oxygen that reaches the organs and tissues it supplies. Medicines can help all types of vasospasms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
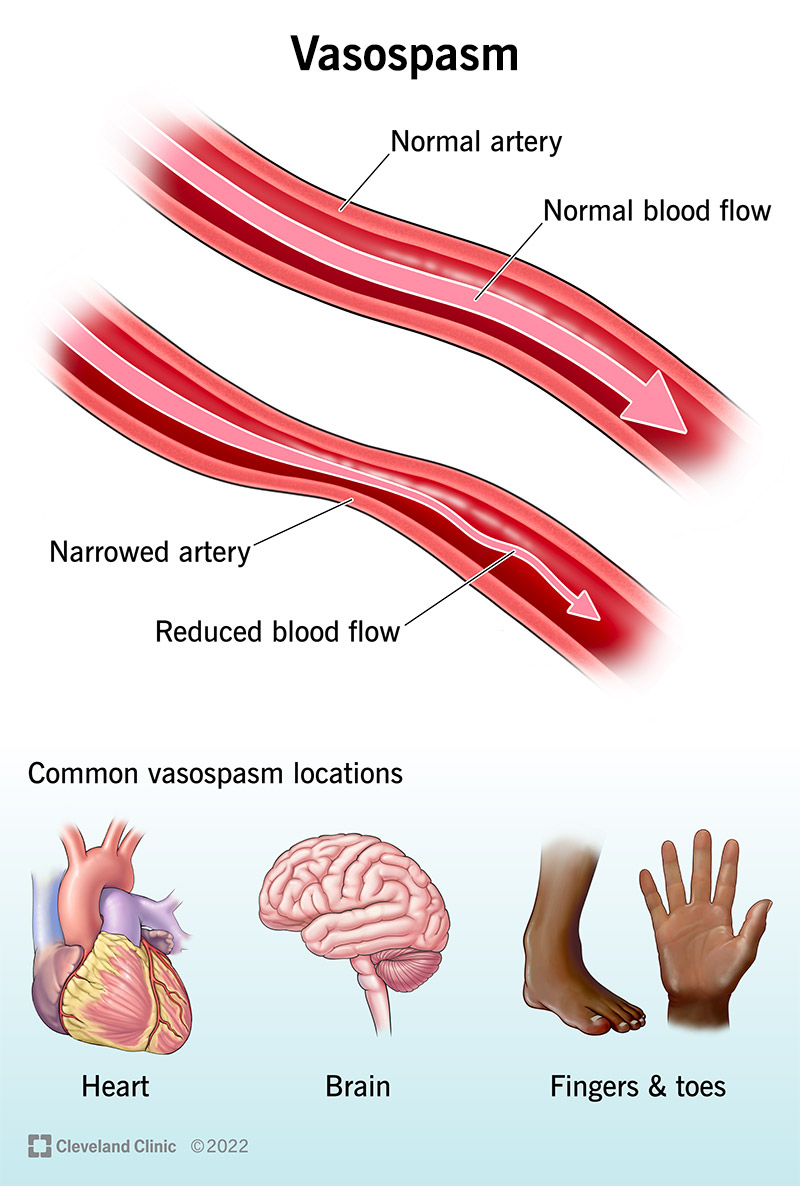
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24825-vasospasm-illustration)
A vasospasm is a lengthy constricting, narrowing or tightening in your artery. This reduces blood flow through the artery, sending less oxygen than normal to nearby tissues.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your arteries expand and contract their muscular walls regularly to help control the pressure of blood moving through them. Because vasospasms last longer than a normal constriction, they can damage the layers of your artery walls. It’s like clenching your fists for too long.
Vasospasm is more likely to happen in abnormal areas of blood vessels (endothelial dysfunction).
During a vasospasm, smooth muscle overreacts to signals to constrict. Normally, these muscles have a temporary response to a signal to tighten an artery wall. During a vasospasm, the muscles constrict longer than they should.
Vasospasms happen in various arteries, but they happen more often in some arteries than others. These include your heart and brain.
A vasospasm’s effects vary depending on where they happen, for example:
An estimated 20% of women may have vasospasm in their nipples during breastfeeding. As many as 50% to 90% of people with an aneurysm rupture in their brain get a vasospasm.
Advertisement
Vasospasm symptoms are different depending on where the vasospasm happens.
These happen at rest, at night, in the early morning and in the cold. Researchers also have linked them to anxiety and depression.
Coronary vasospasm symptoms include:
Cerebral vasospasm symptoms include:
Symptoms of a vasospasm in your finger or toe include:
Symptoms of nipple vasospasm in those who breastfeed include:
Vasospasms in various parts of your body have different causes.
Direct causes aren’t well understood, but conditions and causes that are associated with coronary vasospasm include:
Cerebral vasospasm causes include:
Causes of vasospasms in your fingers and toes include:
Nipple vasospasm causes include:
A provider’s physical exam can be a key part of making their diagnosis, but these tests are important, as well:
Vasospasm treatments vary depending on where in your body the vasospasm is happening.
Treatments for a coronary artery vasospasm include:
Cerebral vasospasm treatments include:
Advertisement
Treatments for vasospasms in fingers or toes include:
Treatments for nipple vasospasms include:
Medicines for treating vasospasms may cause:
Vasospasms that happen in your fingers, toes or nipples may be painful and bothersome. However, they’re not life-threatening.
When a vasospasm happens in your heart or brain, the lack of blood flow to those organs can destroy tissue. This can have a severe impact on how well your heart and brain function.
Heart attacks can happen in less than 5% of cases of coronary vasospasms. However, treatments for heart attacks improve your quality of life.
People who have severe brain vasospasms may be in the hospital for weeks.
Advertisement
Some of the ways to reduce your risk of vasospasms are things that are good for your heart and blood vessel (cardiovascular) health in general, such as:
To prevent a cerebral vasospasm, a provider may:
Keep taking the medicines your healthcare provider prescribed. Contact your provider if your symptoms don’t get better. Avoiding the things that can start a vasospasm may help you prevent them. Seek immediate care if you’re having symptoms of a heart attack.
Different treatments are available for the various kinds of vasospasms that can happen. But for some types of vasospasms, you have the power to make changes that can prevent them. Talk to your provider about making a plan for treating and possibly preventing vasospasms.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Need care fast? Cleveland Clinic’s Express Care and Urgent Care locations treat everything from sprains to sinus infections — no appointment needed.
