Enterocolitis is inflammation in both of your intestines at once. You might have enterocolitis if you have an especially severe reaction to common infections. This usually occurs in infants and the immunocompromised.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Enterocolitis is an inflammation that occurs throughout your intestines. It combines “enteritis,” inflammation of the small intestine, with “colitis,” inflammation of the large intestine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Inflammation in either of your intestines is common, but when it occurs in both, it tends to be more severe. It also tends to affect those with more vulnerable immune systems, especially infants.
Inflammation in your intestines typically affects the inner lining (mucosa). It causes swelling, tenderness and changes to the way your intestines secrete and absorb. This affects your digestion and your poop.
Inflammation is a response from your immune system when something is infecting or injuring your body. Your immune system may also cause general symptoms of illness along with local inflammation.
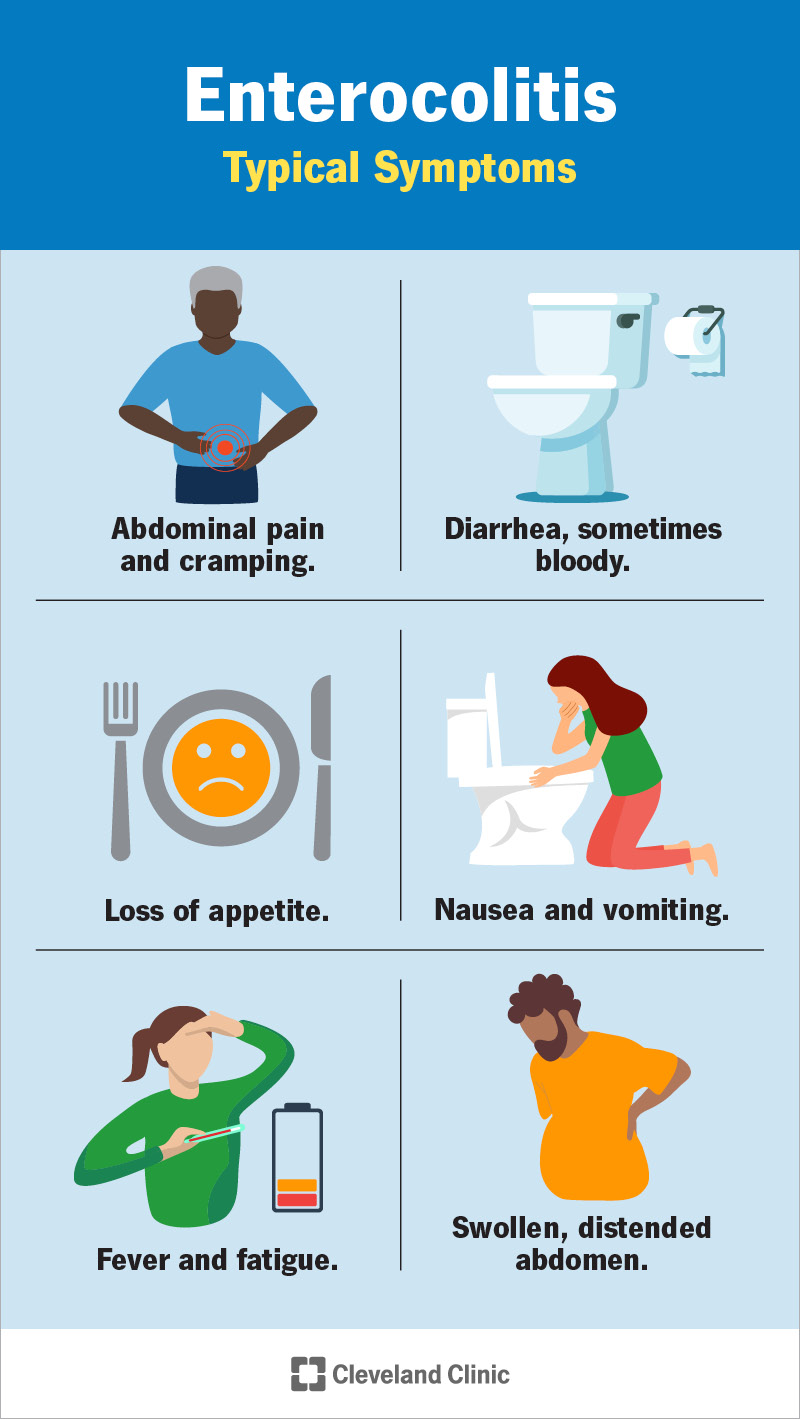
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/24633-enterocolitis)
Typical symptoms of enterocolitis include:
It depends on the cause. Infections, the most common causes, are usually temporary. Your immune system can often defeat them on its own, though sometimes, you might need medication.
Some of the less common causes, such as autoimmune diseases, can be long-lasting. Chronic diseases aren’t curable, but healthcare providers can treat the inflammation separately with medication.
In theory, any of the normal causes of enteritis or colitis could also cause enterocolitis in both intestines. But this would indicate an unusually severe reaction and possibly a more vulnerable immune system.
Advertisement
Common causes of enteritis and colitis include viral infections, such as the stomach flu, parasite infections, like giardiasis, and bacterial infections, such as food poisoning.
Overuse of certain substances, such as alcohol, cocaine and over-the-counter drugs can cause bowel inflammation. Other causes include chronic bowel diseases such as celiac disease and Crohn’s disease.
You’re more likely to get enterocolitis in both intestines if your immune system is not at full strength. Infants and children are more commonly affected, as well as those with chronic illnesses such as HIV.
Healthcare providers have given names to certain types of enterocolitis that come from certain causes. These causes represent trickier infections and diseases that are more likely to affect both intestines.
Specific types include:
Necrotizing enterocolitis (NEC) affects ill and premature infants, who are already immunocompromised. These babies’ intestines react severely when exposed to normal bacteria through feeding. Inflammation and swelling are so severe that the blood supply to their intestinal lining is cut off, causing tissue death. This is what “necrotizing” means.
Doctors aren’t sure what the original cause of inflammation is in NEC. It might be due to the diminished blood supply to these babies’ intestines, or it might be due to bacterial infections that find it easier to take hold when the blood supply is low. Both factors seem to contribute.
Pseudomembranous enterocolitis is also known as antibiotic-associated enterocolitis. It’s caused by a bacterial infection, but also, ironically, by antibiotics. This particular bacterium — Clostridium difficile (C. diff) — tends to infect people who’ve recently taken antibiotics to treat a different infection. Many common antibiotics don’t kill C. diff, but they do kill the other bacteria in your gut that would kill C. diff. This allows C. diff to easily grow out of control.
As it grows, the bacterium releases toxins into your intestinal lining. Some people have a particularly severe reaction to those toxins, which can lead to enterocolitis. This infection is common in hospitals and nursing homes, due to the combination of compromised immune systems, antibiotics use and C. diff’s ability to live for a long time on surfaces.
E. coli infections can cause hemorrhagic enterocolitis. E. coli is a bacterium that commonly and harmlessly lives in our intestines. The danger comes from a particular strain known as enterohemorrhagic E. coli (EHEC), also known as Shiga toxin-producing E. coli (STEC). This strain produces toxins (called Shiga toxins) that adhere to your intestinal lining, causing inflammation and bleeding (hemorrhage.)
Advertisement
“Enterohemorrhagic” means bleeding in your small intestine. Those who react more severely to Shiga toxins may have enterocolitis and bleeding in both intestines. This will cause bloody diarrhea (dysentery.) Hemorrhagic enterocolitis most commonly affects the very young and old.
Food protein-induced enterocolitis syndrome (FPIES) is a food allergy reaction that mostly affects children under two. It causes an inflammatory immune response in their intestinal lining. FPIES is a non-IgE mediated allergy, which makes it different from other allergies you may be familiar with.
Most allergies cause your immune system to produce specific antibodies to the allergen, called IgE antibodies. These antibodies cause an immediate reaction that you may experience as symptoms in your nose, throat, lungs or skin. Non-IgE mediated allergies don’t produce IgE antibodies. Instead, they cause a delayed reaction in your intestines alone, leading to symptoms of enterocolitis.
Hirschsprung-associated enterocolitis is a common and dangerous complication of Hirschprung disease, a birth defect that affects the large intestine. Babies with Hirschprung disease are missing certain cells in the lining of their large intestines, usually in one segment. These cells are involved in the muscle contractions that move poop through the large intestine (peristalsis.)
Advertisement
In the segment where the cells are missing, poop doesn’t continue to move through and builds up, causing a blockage. This blockage creates a breeding ground for bacteria to overgrow. Bacterial overgrowth can spread to both intestines and eventually degrades the intestinal lining, allowing the bacteria to infiltrate the lining. All of these factors may contribute to causing enterocolitis.
Neutropenic enterocolitis affects people experiencing neutropenia, lower-than-normal levels of white blood cells called neutrophils. These are the cells that would normally help protect you from infections. People who have neutropenia are prone to more serious infections that may lead to enterocolitis.
Most people with neutropenic enterocolitis have undergone chemotherapy for blood cancers such as leukemia and lymphoma. These conditions cause neutropenia, and chemotherapy itself contributes to weakening the intestinal mucosa. But it can also occur in people with neutropenia due to other conditions, such as HIV/AIDS and autoimmune diseases.
The signs and symptoms of enteritis, colitis and enterocolitis are similar. A healthcare provider might not know right away which parts of your intestines are affected, but they will suspect inflammation based on your physical signs and symptoms. After that, their job will be to identify the cause. This will allow them to diagnose the specific type of enterocolitis.
Advertisement
Healthcare providers use blood tests, poop tests and imaging tests to look for information about what’s causing your condition. Imaging tests, such as an abdominal ultrasound or CT scan can show evidence of inflammation and possible complications in your bowels. Blood tests and poop tests can help identify specific infections or diseases that may be involved.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_zcy73d6f/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Gut rehabilitation aids those with intestinal failure. It uses IV nutrition, oral rehydration and therapies to restore gut function.
Treatment will be targeted to the cause. Acute treatments might include:
In severe cases, some people need:
Enterocolitis that affects infants, including necrotizing enterocolitis and Hirschsprung-associated enterocolitis, can be life-threatening. However, with timely diagnosis and treatment, most infants recover. Some may continue to have recurring infections or other long-term complications.
Complications can include:
Inflammation in the intestines is common, especially as a response to infection. But when it affects both your small and large intestines, it tends to be more serious. Enterocolitis more often affects people with weaker-than-normal immune systems. This can make it scarier than normal for those affected and their loved ones. But with careful attention and quick response, healthcare providers and treat it before complications arise. If you or a loved one is immunocompromised, stay alert to the risk of enterocolitis.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have issues with your digestive system, you need a team of experts you can trust. Our gastroenterology specialists at Cleveland Clinic can help.
