Myopericarditis is inflammation in two different parts of your heart, but mostly in the protective sac around it (pericardium). Most people get myopericarditis from a virus, but medicines provide relief. Still, recovery can take a few weeks. Long-term effects from it aren’t common.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
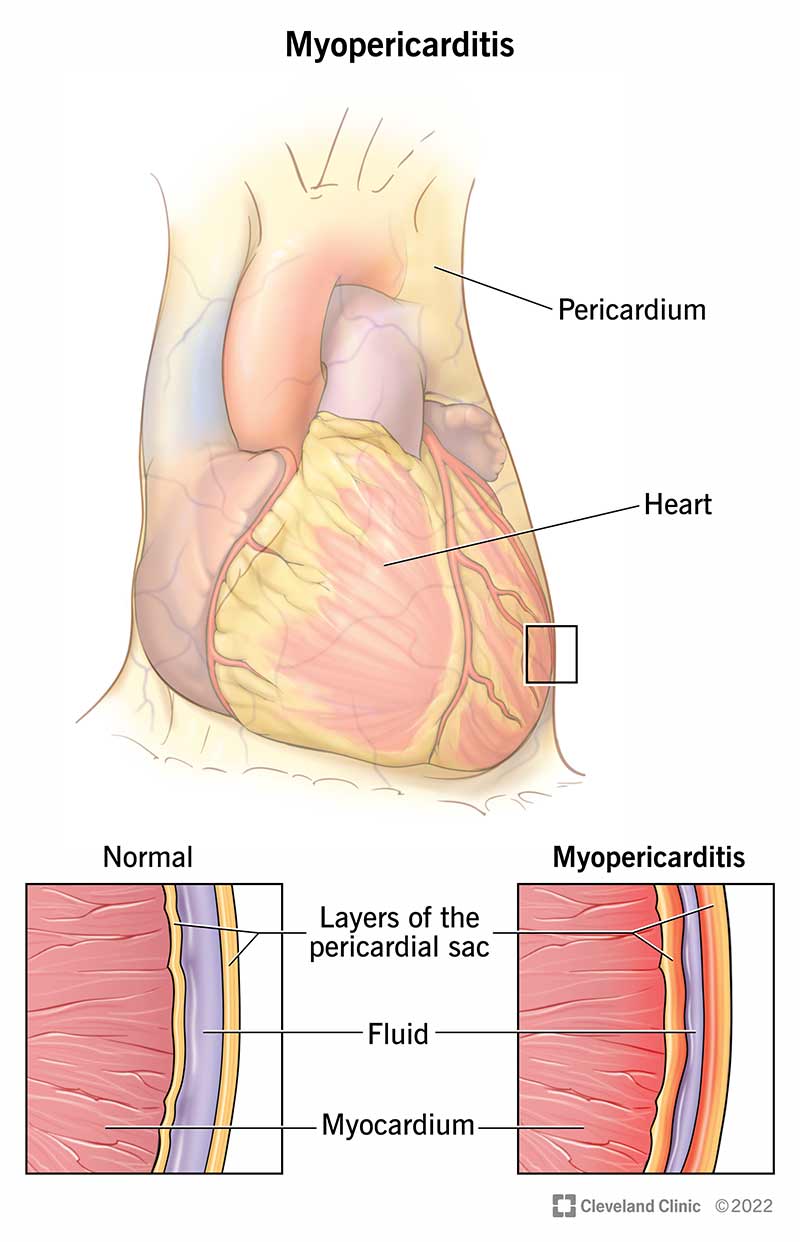
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24579-myopericarditis)
Myopericarditis is a heart condition that affects your heart muscle and the protective sac around your heart.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your heart muscle is your myocardium. An inflamed myocardium is called myocarditis. Your heart’s protective sac, or pericardium, can get inflamed, too. That’s pericarditis.
When both of these happen, but it affects your pericardium more than your heart muscle, it’s myopericarditis. It can be mild to severe. When you have both conditions, but the issue is mostly with your heart muscle, it’s called perimyocarditis.
People with these conditions have similar symptoms, such as:
However, people with myopericarditis more often have abnormal heart rhythms and heart muscle dysfunction. People with pericarditis more often have pericardial effusion.
Myopericarditis symptoms include:
Most of the time, healthcare providers can’t find a definite cause of myopericarditis. However, myopericarditis causes include:
Advertisement
Because providers believe viruses are the most common cause of myopericarditis, having a virus is a risk factor. Viruses that can put you at risk for myopericarditis include herpes, influenza (flu), COVID-19, coxsackie virus, human immunodeficiency virus (HIV) and hepatitis C.
People with myopericarditis are more likely to be male and younger than age 40.
Possible complications of myopericarditis include:
A healthcare provider will do a physical exam and order tests. They may make a myopericarditis diagnosis if you have:
Tests to diagnose myopericarditis include:
Depending on your situation, you may need medicines and/or a procedure for myopericarditis management. Also, a healthcare provider may admit you to the hospital.
Myopericarditis treatments may include:
Possible side effects of the medicines used to treat myopericarditis include:
Complications from pericardiocentesis may include:
Your heart will need time to recover from myopericarditis. If you play sports or your condition affected your heart muscle, your provider may ask you to limit your physical activity for up to six months. You should limit your alcohol intake to a maximum of one drink per day.
Advertisement
You may be taking ibuprofen for days or several weeks. It can take four to six weeks to recover from myopericarditis. You should avoid exerting yourself during that time.
The prognosis for myopericarditis is very good. Most people don’t have complications or long-term effects from the condition. After treatment, myopericarditis usually doesn’t return.
Follow your healthcare provider’s instructions while you recover from myopericarditis. Take medicine as prescribed and go to all follow-up appointments. These visits should happen after one month, six months and one year. These appointments may include:
Contact your provider if you have constrictive pericarditis symptoms, such as:
Questions to ask your doctor may include:
Having chest pain can be unnerving, but getting medical care lets you know what you’re dealing with. With a myopericarditis diagnosis, medicines can help your symptoms. Be sure to keep taking the medicines your provider prescribed. Follow-up appointments are important, too.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether your pericardial disease comes on acutely without warning or is chronic, Cleveland Clinic has the best treatments for this heart condition.
