Uvulopalatopharyngoplasty, or UPPP, is a common surgery healthcare providers use to treat obstructive sleep apnea (OSA). UPPP widens your airway by removing or restructuring tissue in the back of your throat. Your healthcare provider may recommend this surgery if conservative treatments to manage your OSA, like CPAP, haven’t helped.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
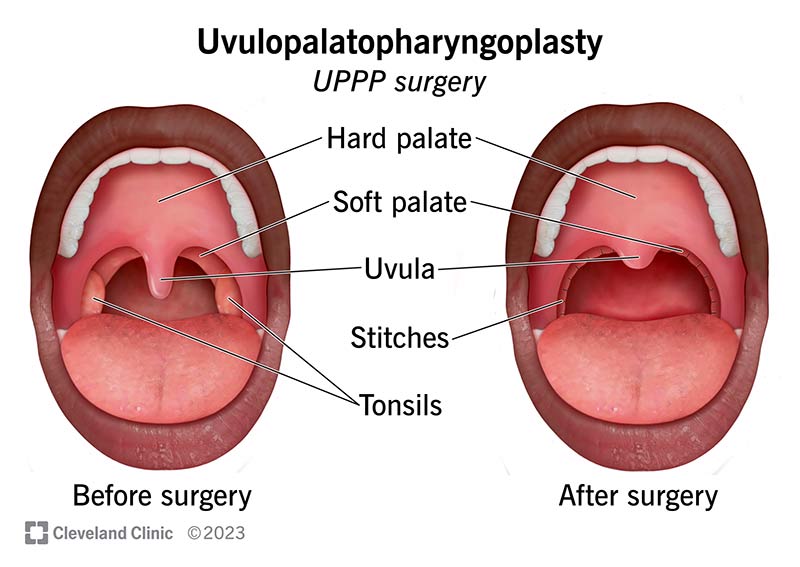
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/25059-uvulopalatopharyngoplasty)
Uvulopalatopharyngoplasty is surgery that opens your airway by removing or reshaping tissue in your throat (pharynx). It’s also called UPPP. You may need UPPP if you have obstructive sleep apnea (OSA).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
UPPP removes tissue blocking your airway so you can breathe (and sleep) more easily. Your surgeon may remove all or part of your:
UPPP may be a standalone procedure. Often, healthcare providers perform UPPP alongside other procedures that also correct structural problems causing sleep apnea. UPPP may help if the tissue collapsing at night is in the back of your throat. You may need different or additional surgeries if you have structural issues in your nasal cavity, farther down your throat or elsewhere.
UPPP may be an option if conservative therapies to manage OSA haven’t worked. First-line treatments include devices that open your airways, like a CPAP machine, and weight loss. Having overweight and obesity are risk factors for OSA.
Research has shown that uvulopalatopharyngoplasty provides the most benefit based on the anatomy of a person’s mouth and throat and their weight. Healthcare providers use a staging system based on these characteristics to determine who is a good candidate for UPPP.
Advertisement
Providers consider:
Providers classify potential candidates for UPPP into Stages 1, 2 or 3. People who are Stage 1 will likely experience symptom improvement following UPPP. People who are Stage 2 and 3 are less likely to benefit from UPPP.
Ask your healthcare provider about the factors that play a role in determining whether you’re a good candidate for this surgery.
Your healthcare provider will review the steps you need to take to prepare for UPPP. Before surgery:
During surgery:
Surgery may take up to two hours, depending on which structures your healthcare provider removes or restructures. Timing also depends on whether you’ll need additional procedures to address other structural issues contributing to your sleep apnea.
You may be discharged the same day or possibly stay in the hospital for one night. Your care team will monitor your vital signs closely. You’ll get to go home once your breathing has stabilized and you can safely swallow.
Your provider will work with you to manage pain during recovery. Before you leave the hospital, they’ll prescribe pain medicines you’ll take at home.
Advertisement
UPPP can help you breathe easier so you’re able to sleep at night. It can help you manage obstructive sleep apnea (OSA) and can reduce related symptoms like excessive snoring.
UPPP is successful when it’s performed on people who are good candidates for this procedure.
UPPP wasn’t as successful when healthcare providers first started performing the procedure in 1981. Often, symptoms improved after surgery only to gradually return. Results improved once healthcare providers began staging people to identify the best candidates for surgery. According to research, 80.6% of people who are Stage 1 experience symptom improvement after UPPP.
UPPP eliminates sleep apnea entirely in some people. UPPP improves sleep apnea symptoms for others, but they still need to use a CPAP machine. Your response to treatment depends on your anatomy and other factors that you should discuss with your provider.
All surgeries come with risks like infection and bleeding. You may be allergic to the anesthesia. Complications unique to UPPP include:
Advertisement
Discuss risks and potential complications with your healthcare provider before surgery so you know how to prepare.
Recovery may take two to four weeks or even longer, depending on how extensive your surgery was. Most people need to take time off from work or school while recovering.
Follow your healthcare provider’s instructions about how to care for yourself after surgery. They can advise you on what symptoms are related to healing and which symptoms may be signs of a complication. Follow their advice on when it’s safe to use CPAP following surgery if you continue to use it.
Contact your healthcare provider if uvulopalatopharyngoplasty doesn’t improve your symptoms or if you notice signs of complications. Call if you notice:
Advertisement
See a healthcare provider immediately or visit the ER if you have bleeding.
Uvulopalatopharyngoplasty, or UPPP, is a common surgery to treat obstructive sleep apnea (OSA). It may be an option if other methods to manage your OSA haven’t helped. Ask your healthcare provider about treatment outcomes based on your unique diagnosis, including whether you’ll need to continue using a CPAP. Understanding your treatment goals will help you throughout the recovery period and beyond.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Obstructive sleep apnea can keep you from the getting the good night’s rest you need. Cleveland Clinic’s experts can create a treatment plan that helps.
