A pheochromocytoma is a rare but treatable tumor that forms in the middle of your adrenal gland. In most cases, the tumor is benign, but it can be malignant (cancer). Symptoms include high blood pressure and headaches, though you could experience no symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
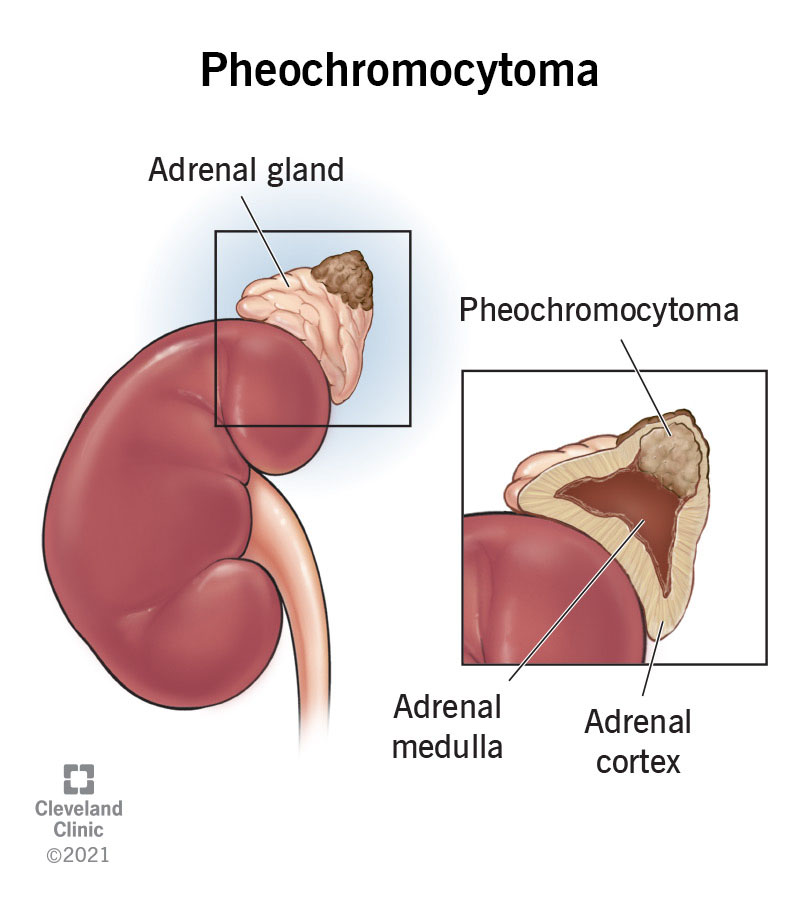
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23373-pheochromocytoma)
A pheochromocytoma (pronounced FEE-oh-KROH-moh-sy-TOH-muh) is a rare tumor that forms in the center of one or both of your adrenal glands (adrenal medulla). The tumor is made of a certain type of cell called a chromaffin cell, which produce and release the hormones that cause the “fight or flight” response.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Usually, pheochromocytoma affects only one adrenal gland, but it can affect both glands. Sometimes there’s more than one tumor in one adrenal gland.
Most pheochromocytomas are benign (not cancerous). Approximately 10% to 15% of pheochromocytomas may be malignant (cancerous). There's no standard staging system for pheochromocytoma if it’s cancerous. Instead, it’s described as the following:
You have two adrenal glands, one on top of each kidney in the back of your upper abdomen. They are part of your endocrine system. Each adrenal gland has two parts. The outer layer of your adrenal gland is called your adrenal cortex. The center of your adrenal gland is called your adrenal medulla.
Your adrenal medullae make hormones called catecholamines that help regulate the following important bodily functions and aspects:
Advertisement
The primary catecholamines include:
Sometimes a pheochromocytoma can release extra adrenaline and noradrenaline into your blood, causing certain symptoms.
Pheochromocytoma and paraganglioma are both rare tumors that come from the same type of cells known as chromaffin cells.
Pheochromocytoma is a tumor that forms in the center of your adrenal gland (adrenal medulla), and paragangliomas form outside your adrenal gland.
Anyone at any age can get a pheochromocytoma, but they occur most often in people between 30 and 50 years of age. Approximately 10% of cases occur in children.
Pheochromocytomas are rare tumors. The true number of pheochromocytoma cases is unknown since many people with pheochromocytomas don’t have symptoms and go undiagnosed. Less than 1% of people who have high blood pressure have a pheochromocytoma.
Signs and symptoms of pheochromocytoma happen when the tumor releases too much adrenaline (epinephrine) or noradrenaline (norepinephrine) into your blood. However, some pheochromocytoma tumors don’t make extra adrenaline or noradrenaline and don’t cause symptoms (are asymptomatic).
Common symptoms of pheochromocytoma include:
Less common symptoms of pheochromocytoma include:
You may experience signs and symptoms of pheochromocytoma after certain events, including:
A person with a pheochromocytoma could have sustained high blood pressure (the most common symptom of pheochromocytoma) or it may come and go.
People with pheochromocytomas may also experience paroxysmal “attacks,” which are chronic episodes of high blood pressure that often lead to headaches, irregular heartbeats (palpitations) and excessive sweating (diaphoresis). These episodes can happen anywhere from several times a day to a couple of times a month.
In most cases of pheochromocytoma, the exact cause is unknown, and it occurs randomly.
Advertisement
Approximately 25% to 35% of people who have pheochromocytoma have a hereditary condition (passed through the family) that’s linked to pheochromocytoma, including:
Pheochromocytomas may also be caused by mutations (changes) of one of at least 10 different genes.
Since pheochromocytoma is a rare tumor and is sometimes asymptomatic, it can be difficult to diagnose. Healthcare providers sometimes find pheochromocytomas when a test or procedure is done for another reason.
A healthcare provider may suspect a diagnosis of pheochromocytoma after reviewing the following factors:
Your healthcare provider may use the following tests and procedures to diagnose pheochromocytoma:
Advertisement
After your provider has diagnosed pheochromocytoma, they’ll likely perform additional tests to see if the tumor is benign or malignant and if it has spread to other parts of your body.
Advertisement
If you’re diagnosed with pheochromocytoma, your provider may recommend genetic counseling to find out your risk for having an inherited syndrome and other related cancers.
Your healthcare provider may recommend genetic testing if any of the following situations apply to you:
If your genetic counselor finds certain gene changes in your testing results, they'll likely recommend that your family members who are at risk but do not have signs or symptoms be tested as well.
The best treatment option is surgery, when feasible.
Treatment options for pheochromocytoma depend on several factors, including:
If you have pheochromocytoma that causes symptoms due to excess adrenal hormones, your healthcare provider will likely recommend medication to manage the symptoms. Medications may include:
Treatment options for pheochromocytoma include:
Together, you and your healthcare team will determine a treatment plan that works best for you and your situation.
Surgery is the main form of treatment for pheochromocytoma. Approximately 90% of pheochromocytomas are successfully removed by surgery.
If you have a pheochromocytoma, your provider may recommend a type of surgery called adrenalectomy to remove one or both of your adrenal glands. During the surgery, your surgeon will check the surrounding tissue and lymph nodes to see if the tumor has spread. If it has, your surgeon will remove the affected tissue(s) as well, if possible.
After surgery, your provider will check the catecholamine levels in your blood or urine. Normal catecholamine levels are a sign that all the pheochromocytoma cells were removed.
If your surgeon removes both of your adrenal glands, you’ll need life-long hormone therapy to replace hormones made by your adrenal glands.
Radiation therapy is a cancer treatment that focuses strong beams of energy to destroy cancer cells or keep them from growing while sparing as much surrounding healthy tissue as possible.
There are two types of radiation therapy:
The type of radiation therapy your provider may recommend depends on whether your cancer is localized, regional, metastatic or recurrent. Providers most often use external radiation therapy and/or 131I-MIBG therapy to treat malignant pheochromocytoma. 131I-MIBG is a radioactive substance infusion that collects in certain kinds of tumor cells, killing them with the radiation that it gives off.
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells by killing the cells or by preventing them from dividing and multiplying. Chemotherapy is usually given intravenously through a vein (intravenously). It’s usually an effective treatment, but it can cause side effects.
Ablation therapy is a minimally invasive treatment option that uses very high or very low temperatures to destroy tumors. Ablation therapies that can help kill cancer cells and abnormal cells include:
Embolization therapy is a pheochromocytoma treatment that blocks the artery leading to your adrenal gland. Blocking the blood flow to your adrenal glands helps kill the cancer cells that are growing there.
Targeted therapy is a treatment option that uses medications or other substances to attack specific cancer cells without harming healthy cells. Healthcare providers use targeted therapies to treat metastatic and recurrent pheochromocytoma.
Researchers are currently studying sunitinib, a type of tyrosine kinase inhibitor, for the treatment of metastatic pheochromocytoma. Tyrosine kinase inhibitor therapy is a type of targeted therapy that prevents tumors from growing.
The prognosis (outlook) for pheochromocytoma is usually good if it’s treated. Approximately 90% of pheochromocytomas are successfully removed by surgery.
If pheochromocytomas are left untreated, they can potentially cause serious, life-threatening complications, including:
Some people with a pheochromocytoma may also be at risk of developing a stroke or heart attack (myocardial infarction).
Unfortunately, you can’t prevent developing a pheochromocytoma. However, if you’re at risk for developing a pheochromocytoma due to certain inherited syndromes and genes, genetic counseling can help screen for pheochromocytoma and potentially help you catch it in its early phases.
Talk to your healthcare provider if you have any first-degree relatives (siblings and parents) that have been diagnosed with pheochromocytoma and/or any of the following genetic conditions:
If you’ve been diagnosed with a pheochromocytoma and are experiencing concerning symptoms, contact your healthcare provider.
If you’re experiencing symptoms of pheochromocytoma, such as high blood pressure and headaches, talk to your provider. Even though pheochromocytoma is rare and the likelihood of having it is low, it’s important to treat high blood pressure.
If you’ve recently found out that one of your first-degree relatives (siblings and parents) has a genetic syndrome, such as multiple endocrine neoplasia 2 syndrome or von Hippel-Lindau (VHL) disease, that puts you at a higher risk of developing pheochromocytoma. You should contact your provider about genetic testing.
If you’ve been diagnosed with a pheochromocytoma, it may be helpful to ask your healthcare provider the following questions:
Pheochromocytoma is a rare tumor. The good news is that it’s often benign and treatable. While most pheochromocytoma cases have an unknown cause, there’s a significant link to certain inherited conditions. If you or one of your first-degree relatives have been diagnosed with a pheochromocytoma, it’s important to go through genetic testing to make sure you don’t have a genetic condition that could potentially cause other medical issues. If you have any questions about your risk of developing a pheochromocytoma, talk to your healthcare provider. They’re there to help you.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When your hormones are out of balance, so are you. Cleveland Clinic experts can diagnose and treat some adrenal disorders to help you feel like yourself again.
