A pseudoaneurysm is a pooling of blood that develops from an injury to your artery or, rarely, your heart. The most common type is a femoral pseudoaneurysm (in the groin area). This is a possible complication of catheter-based procedures. Pseudoaneurysms also affect other arteries, like those in your chest and belly. They’re usually treatable.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
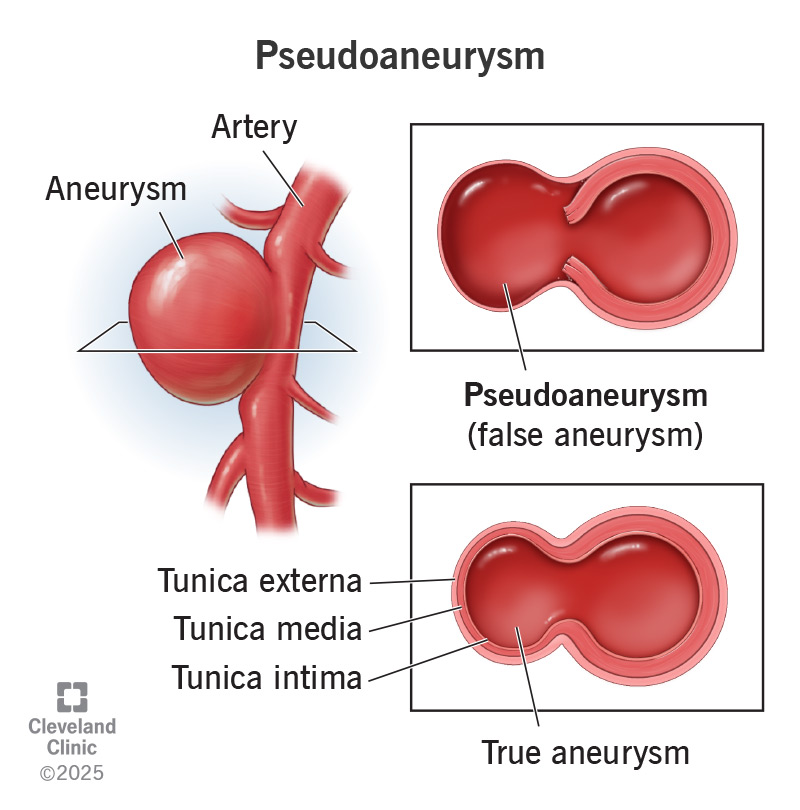
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23250-pseudoaneurysm)
A pseudoaneurysm (also called a false aneurysm) is contained bleeding from an injury to your artery. It looks like a round bulge that sticks out from one side of your artery. The blood collects within a “wall” that keeps it from leaking into nearby tissues.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You might wonder what’s “pseudo,” or false, about this condition. A pseudoaneurysm is very real — and it can be serious if its wall ruptures. But it’s “false” in the sense that it doesn’t involve all three layers of your artery wall. A “true” aneurysm involves all three layers. Those layers, together, serve as the aneurysm’s wall.
A pseudoaneurysm, on the other hand, only uses one or two layers of your artery wall for its own wall. The rest of its wall is made of tissue that forms when the artery is injured. Its wall is weaker than an aneurysm’s wall.
Some pseudoaneurysms are harmless and go away on their own. Others are more serious. If they rupture, they can cause severe complications or death. It’s important to know the causes and symptoms so you can seek medical care when needed.
Healthcare providers divide these false aneurysms into different types based on their location. Here are some examples:
Advertisement
Pseudoaneurysm symptoms include:
Symptoms of left ventricular and aortic pseudoaneurysms are different. They include:
Pseudoaneurysms can develop if there’s damage to an artery. The most common causes of such damage include:
Injuries to your arteries can also cause hematomas. But a hematoma is a pooling of blood that doesn’t have walls around it, as a pseudoaneurysm does. Think of a hematoma like a bruise.
Without treatment, this can lead to:
Some pseudoaneurysms — especially those that form in your heart — can be fatal. Early diagnosis and treatment can be lifesaving.
Your provider will discuss your symptoms and give you a physical exam. The size and location of the pseudoaneurysm determine what they look for and the tests they use.
For example, if your provider suspects a femoral pseudoaneurysm, they’ll check for:
Your provider may also perform a duplex ultrasound. This is a common method for checking blood flow in your arteries and veins. This painless test can also check the size and location of the pseudoaneurysm.
If your provider suspects a left ventricular or aortic pseudoaneurysm, they’ll do imaging tests. These help your provider see any issues. Possible tests include:
Treatment for a pseudoaneurysm depends on its location and size. Options include:
Advertisement
Your provider will tell you which treatment is best for your case. They’ll also explain the benefits and risks.
Call your healthcare provider if:
Call 911 (or your local emergency service number) if you have a known pseudoaneurysm and develop sudden, significant pain in your chest, back or abdomen.
A pseudoaneurysm is dangerous if it ruptures. It can cause internal bleeding and, possibly, death. But when caught early and treated, pseudoaneurysms are easily manageable. You may need follow-up visits with your provider after treatment.
Learning you have a pseudoaneurysm can be scary and unexpected. But with quick treatment, there’s a good chance you can recover and carry on with life as normal. The key is getting diagnosed early when symptoms first start.
If you’re having a catheter-based procedure, talk to your provider beforehand about the risks. Pseudoaneurysms are rare complications of such procedures, but they can happen. Knowing what your provider can do to lower the risk — or treat a pseudoaneurysm if it happens — may help put your mind at ease.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Vascular disease may affect your life in big and small ways. Cleveland Clinic’s specialists treat the many types of vascular disease so you can focus on living.
