Prolactinoma is a noncancerous tumor that makes extra prolactin. It can cause symptoms like infertility, irregular periods and milky nipple discharge. The good news is that prolactinoma is often treatable with medication and/or surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Prolactinoma is a generally benign (noncancerous) tumor that forms in your pituitary gland and makes more prolactin — a hormone — than you need. About 50% of pituitary tumor (pituitary adenoma) cases are prolactinomas, making them the most common type of pituitary tumor.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Prolactin is mainly responsible for the development of mammary glands within breast tissue and lactation. It contributes to several other bodily processes as well. Prolactinomas cause higher-than-normal levels of prolactin in your blood (hyperprolactinemia), resulting in infertility and other issues.
The thought of having a tumor so close to your brain can be unsettling. You may breathe a little easier knowing that prolactinomas aren’t life-threatening. But they can cause unwanted health issues, so it’s important to seek care if you develop symptoms.
There are two main types of prolactinomas based on their size:
Among people with prolactinomas, as many as 60% of males have macroprolactinomas, while 90% of females have microprolactinomas.
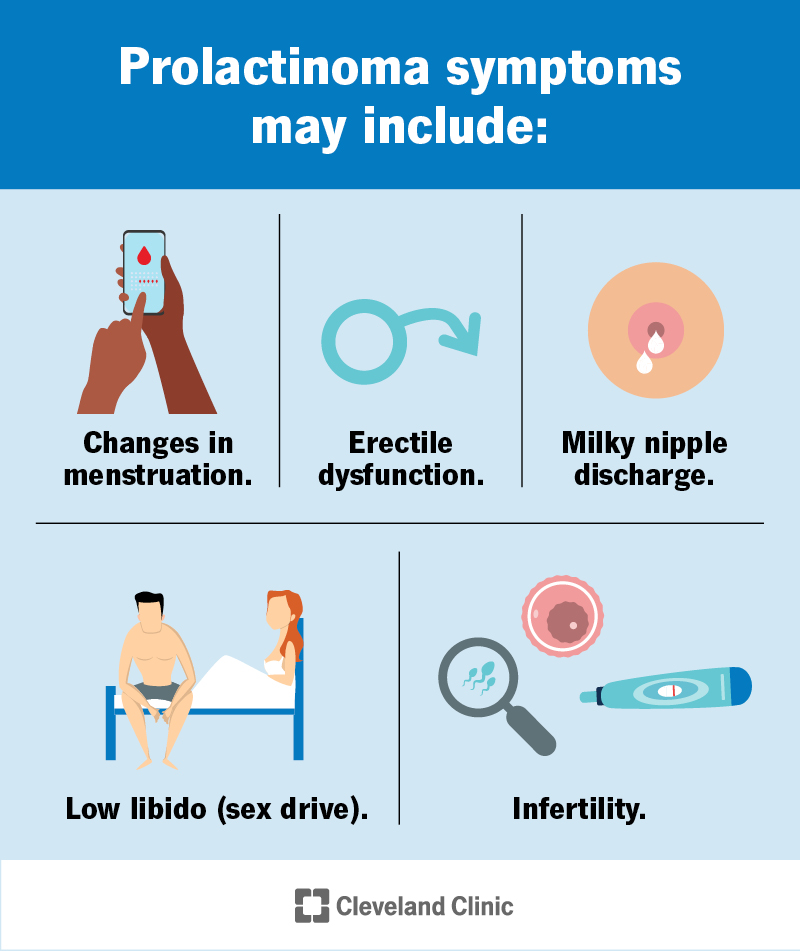
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22007-prolactinoma)
The symptoms of prolactinoma can vary depending on how much prolactin it produces and its size.
Symptoms of prolactinoma in adults include:
Advertisement
Left untreated, high prolactin levels can also lead to osteopenia and/or osteoporosis.
If the prolactinoma is large (macroprolactinoma), it may also cause the following symptoms:
Females often notice symptoms earlier due to changes in their periods or milky nipple discharge. But if you're hormonal medications — like birth control pills or hormone replacement therapy — you may not experience these symptoms.
Females who've reached menopause and males often have a delayed diagnosis.
It’s very rare for children to develop a prolactinoma. But if they do, prolactinomas typically cause delayed puberty.
Researchers don’t know the exact cause of prolactinoma. Many cases happen randomly (sporadically). But certain genetic conditions can increase your risk for prolactinoma, including:
Your healthcare provider will ask about your symptoms and medical history and do a physical exam. If you have milky nipple discharge, they may do a breast exam. They’ll likely recommend one or more of the following tests to diagnose prolactinoma:
If you receive a prolactinoma diagnosis, your provider may recommend additional blood tests to check the levels of other pituitary hormones. If you have a large prolactinoma, your provider may recommend an eye exam to see if it’s affecting your vision.
Prolactinomas are often highly treatable. Healthcare providers usually prescribe medication to treat them. In rare cases, your provider may recommend surgery or radiation therapy.
Advertisement
Medications called dopamine agonists are often very effective in shrinking prolactinoma tumors. They can also return your prolactin level to a healthy range.
The two dopamine agonists that healthcare providers prescribe to treat prolactinomas are cabergoline and bromocriptine. Cabergoline is often the first-choice medication because it’s more effective than bromocriptine and has fewer side effects.
Common side effects of dopamine agonists include nausea, vomiting and dizziness.
You’ll likely have to take either of these medications for at least two years to prevent the tumor from growing back, especially if it’s large. After two years, your provider may slowly reduce your dosage and then stop the medication if your prolactin levels are normal and the tumor is no longer visible.
Although it’s rare, you may need to have surgery to treat prolactinoma for any of the following reasons:
Together, you and your healthcare provider will decide if surgery is the best option for you. Surgeons use two types of surgeries to remove prolactinomas, including:
Advertisement
As with all surgeries, there are possible complications and risks associated with prolactinoma surgery. Your provider will go over these risks with you.
Radiation therapy is a rare third option for treating prolactinomas if medications and/or surgery don’t work to reduce your prolactin levels. Depending on the size and location of the tumor, you may receive one radiation dose or multiple doses over several weeks.
The prognosis (outlook) for someone with prolactinoma is generally good. Medication (dopamine agonists) shrinks small prolactinoma tumors and brings prolactin levels back to normal for 4 out of 5 people receiving this treatment.
Prolactinoma surgery is also often successful. When an experienced surgeon performs the surgery, it corrects prolactin levels in about 90% of people with small tumors and in 50% of those who have large tumors. If you have a large tumor that can only be partially removed, medications can often return your prolactin levels to a normal range after surgery.
Advertisement
Unfortunately, there’s nothing you can do to prevent developing prolactinoma. A known risk factor is having an inherited (passed through your biological family) condition called multiple endocrine neoplasia (MEN) type 1.
If you have a first-degree relative (biological sibling or parent) who has this condition, you may want to get genetic counseling to check if you have it as well. This may help screen for and catch prolactinoma in its early phases.
If you’re taking medication to treat prolactinoma, you’ll likely be on it for a long time — typically, at least two years. If you’re taking medication, you’ll likely need to see your healthcare provider regularly to monitor the tumor and your prolactin levels.
If you experience concerning symptoms after starting medication, contact your provider.
Finding out you have a tumor can be scary. The good news is that prolactinomas are almost always benign (noncancerous) and highly treatable — usually with medication. Know that your healthcare team will be by your side to answer any questions and ease any concerns.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Hormonal conditions can be tricky to find and complicated to treat. The experts in endocrinology at Cleveland Clinic are here to provide the best care.
