Ear infections (acute otitis media) occur when a virus or bacteria infects the space behind your child’s eardrum. Symptoms include ear pain that may cause your infant or toddler to be especially fussy or irritable. Often, ear infections clear on their own. Sometimes, children need antibiotics, pain-relieving medications or ear tubes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
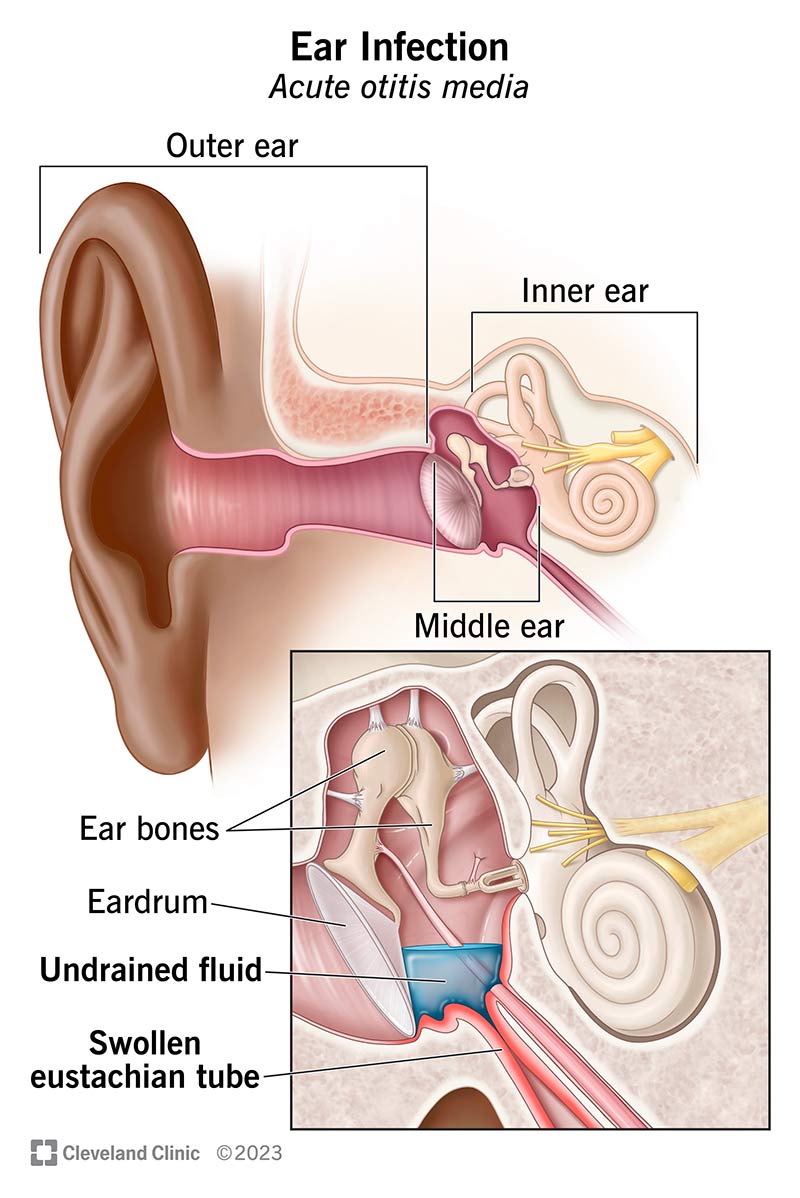
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/8613-ear-infection)
An ear infection, also called acute otitis media, is a sudden infection in your middle ear. The middle ear is the air-filled space between your eardrum and inner ear. It houses the delicate bones that transmit sound vibrations from your eardrum to your inner ear so you can hear.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Eustachian tubes are canals that connect your middle ear to the back of your throat. They regulate air pressure in your ear and prevent fluid from accumulating in your middle ear space.
If a eustachian tube doesn’t function well, fluid has a hard time draining from your middle ear space and can cause muffled hearing. Ear infections (from viruses and bacteria) also cause middle ear fluid. In these cases, the middle ear fluid is infected and often causes discomfort in addition to muffled hearing.
Middle ear infections are the most common childhood illness other than colds. Ear infections occur most often in children between 6 months and 2 years. They’re common until age 8.
Older children and adults can get ear infections, too, but they don’t happen nearly as often as in young children.
Children get ear infections more often than adults because:
Symptoms of an ear infection often begin after a cold. They include:
Advertisement
Don’t place anything in your ear canal if you have drainage from your ear. An item touching a torn (ruptured) eardrum can cause more damage.
Since small children and infants can’t always communicate their symptoms, it’s important to recognize the signs. A child with an ear infection may:
Bacteria and viruses cause ear infections. Often, ear infections begin after a cold or another upper respiratory infection. The germs travel into your middle ear through the eustachian tube. Once inside, the virus or bacteria can cause your eustachian tubes to swell. The swelling can cause the tube to become blocked, leading to poor eustachian tube function and infected fluid in your middle ear.
Ear infections aren’t contagious, but the virus and/or bacteria causing the infection are. Multiple types of bacteria and viruses cause ear infections, including ones that cause colds and the flu.
Risk factors for ear infections include:
Most ear infections don’t cause long-term issues. When complications happen, they’re usually related to repeated or ongoing ear infections. Complications include:
Advertisement
Most healthcare providers can tell if your child has an ear infection based on their symptoms, a physical exam to check for signs of a cold and an ear exam. For the ear exam, your child’s healthcare provider will view your child’s eardrum using a lighted instrument called an otoscope. An inflamed, swollen or red eardrum is a sign of an ear infection.
Advertisement
Your child’s provider may use a pneumatic otoscope to check for fluid in your child’s middle ear. A pneumatic otoscope blows a puff of air at the eardrum, which should cause it to move back and forth. It won’t move easily if there’s fluid inside your child’s ear.
Your child may need other tests, including:
Treatment depends on many factors, including:
Advertisement
Often, ear infections heal without treatment. Your provider may monitor your child’s condition to see if it improves before prescribing treatments. Your child may need antibiotics or surgery for infections that don’t go away. In the meantime, pain medicines can help with symptoms like ear pain.
Your child may need antibiotics if bacteria are causing the ear infection. Healthcare providers may wait up to three days before prescribing antibiotics to see if a mild infection clears on its own. If an infection is severe, your child may need to start antibiotics immediately.
The American Academy of Pediatrics provides guidelines on when a child should receive antibiotics and when it’s better to observe. Factors include your child’s age, the severity of their infection and their temperature. The table below summarizes the recommendations.
American Academy of Pediatrics Treatment Guide for Acute Otitis Media (AOM)
| Child’s Age | Severity of AOM / Temperature | Treatment |
|---|---|---|
| 6 months and older; in one or both ears. | Moderate to severe for at least 48 hours or temp of 102.2 degrees F (39 degrees C) or higher. | Treat with antibiotics. |
| 6 months through 23 months; in both ears. | Mild for less than 48 hours and temp less than 102.2 degrees F (39 degrees C). | Treat with antibiotics. |
| 6 months to 23 months; in one ear. | Mild for less than 48 hours and temp less than 102.2 degrees F (39 degrees C). | Treat with antibiotics OR observe. If observe, start antibiotics if the child’s condition worsens or doesn’t improve within 48 to 72 hours of start of symptoms. |
| 24 months or older; in one or both ears. | Mild for less than 48 hours and temp less than 102.2 degrees F (39 degrees C). | Treat with antibiotics OR observe. If observe, start antibiotics if the child’s condition worsens or doesn’t improve within 48 to 72 hours of start of symptoms. |
| Child’s Age | ||
| 6 months and older; in one or both ears. | ||
| Severity of AOM / Temperature | ||
| Moderate to severe for at least 48 hours or temp of 102.2 degrees F (39 degrees C) or higher. | ||
| Treatment | ||
| Treat with antibiotics. | ||
| 6 months through 23 months; in both ears. | ||
| Severity of AOM / Temperature | ||
| Mild for less than 48 hours and temp less than 102.2 degrees F (39 degrees C). | ||
| Treatment | ||
| Treat with antibiotics. | ||
| 6 months to 23 months; in one ear. | ||
| Severity of AOM / Temperature | ||
| Mild for less than 48 hours and temp less than 102.2 degrees F (39 degrees C). | ||
| Treatment | ||
| Treat with antibiotics OR observe. If observe, start antibiotics if the child’s condition worsens or doesn’t improve within 48 to 72 hours of start of symptoms. | ||
| 24 months or older; in one or both ears. | ||
| Severity of AOM / Temperature | ||
| Mild for less than 48 hours and temp less than 102.2 degrees F (39 degrees C). | ||
| Treatment | ||
| Treat with antibiotics OR observe. If observe, start antibiotics if the child’s condition worsens or doesn’t improve within 48 to 72 hours of start of symptoms. |
Even if symptoms improve, don’t stop taking the medicine until your provider tells you to stop. The infection can return if your child doesn’t take all antibiotics as prescribed.
Your healthcare provider may recommend over-the-counter (OTC) medicines, such as acetaminophen (Tylenol®) or ibuprofen (Advil®, Motrin®), to relieve pain and reduce fever. They may prescribe pain-relieving ear drops. Follow your provider’s instructions about what medicines are safe for your child.
Never give aspirin to children. Aspirin can cause a life-threatening condition called Reye’s syndrome.
Your child may need ear tubes if they experience frequent ear infections, infections that don’t improve with antibiotics or hearing loss related to fluid buildup. An ear, nose and throat (ENT) specialist places the tubes during a tympanostomy. It’s a short (approximately 10-minute) procedure. Your child can go home that same day.
During a tympanostomy, a provider inserts a small metal or plastic tube into a tiny incision (cut) in your child’s eardrum. The procedure to perforate (pierce a hole into) and drain the eardrum is called a myringotomy. Once the tubes are in place, they let air into the middle ear and allow fluid to drain.
The tube usually stays in place for 12 to 18 months. It may fall out on its own, or your child may need surgery to remove it. Once the tubes are gone, the hole in your child’s eardrum will heal and close.
Yes, most infections go away on their own. This is why your healthcare provider may wait before prescribing medications like antibiotics. In the meantime, pain relievers can help with symptoms like ear pain.
Depending on your child’s age, symptoms and temperature, they may need antibiotics to heal. If your child has ongoing or frequent infections, or if fluid remains in the middle ear and puts their hearing at risk, your child may need ear tubes. Follow your healthcare provider’s guidance about caring for your child.
Children can return to school or daycare when their fever is gone.
Here are some ways to reduce your or your child’s risk of ear infections:
Call your healthcare provider immediately if:
Call your healthcare provider during office hours if:
No, you don’t need to cover their ears to go outside.
Swimming is OK as long as your child doesn’t have a tear (perforation) in their eardrum or drainage from their ear.
Air travel or a trip to the mountains is safe, although you may feel temporary pain during takeoff and landing when flying. Swallowing fluids or chewing gum during descent can help with the pain. If your small child has an ear infection, have them suck on a pacifier to relieve discomfort during air travel.
Contact your child’s pediatrician if they show signs of an ear infection and their condition doesn’t improve within two to three days. Often, ear infections get better without treatment. Depending on your child’s age and symptoms, they may need antibiotics. Your child’s healthcare provider can recommend pain relievers for your child as their body works through the illness.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Need care fast? Cleveland Clinic’s Express Care and Urgent Care locations treat everything from sprains to sinus infections — no appointment needed.
