Endometriosis causes tissue that is similar to the lining of the uterus to grow in other places where it doesn’t belong. It can cause pelvic pain and heavy periods, as well as fertility issues. Treatment for endometriosis involves medication, surgery or a combination of both.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
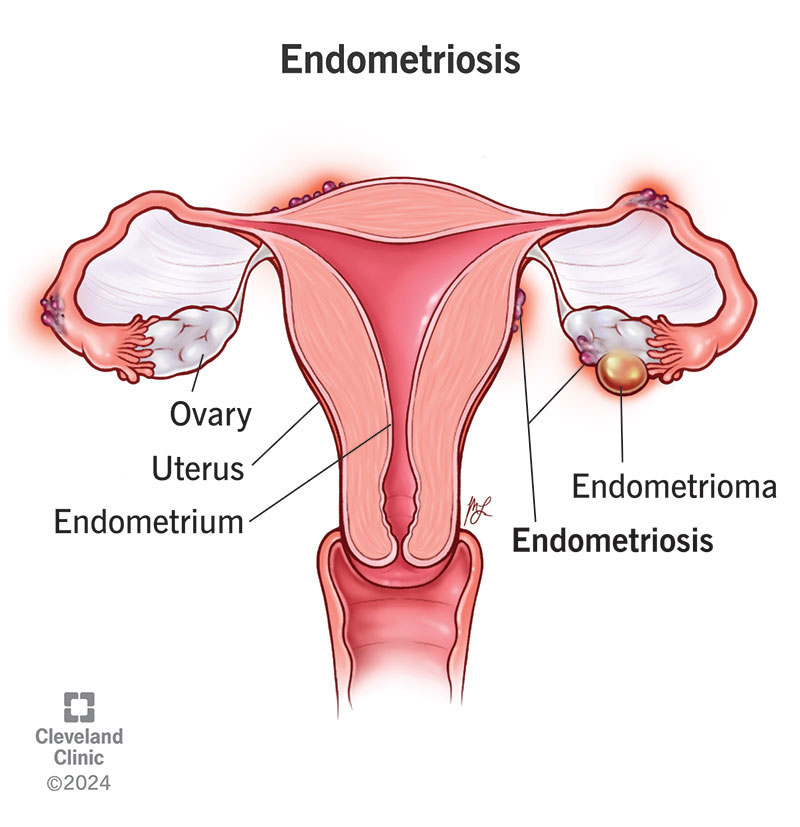
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/10857-endometriosis)
Endometriosis is a condition where tissue that is similar to the lining of your uterus grows on other parts of your body. When this tissue grows in the wrong places, it can cause painful symptoms that can impact not only your menstrual cycle but also your daily life. Some people with endometriosis have trouble getting pregnant due to scarring and fallopian tube blockage as well.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Some of the most common places you can develop endometriosis include the:
Less common places include your:
Endometriosis is a common condition that affects about 1 in 10 females worldwide. Healthcare providers most often diagnose it in people in their 20s and 30s. The symptoms of endometriosis are often manageable with treatment.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_taavjiqd/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
The most common signs of endometriosis.
There are many symptoms of endometriosis, but the most common is pelvic pain. This pain can be intense or mild. Symptoms often feel worse just before and during your period due to inflammation brought on by the hormonal changes that occur at that time.
Symptoms of endometriosis include:
You can also have no symptoms of endometriosis. Sometimes, you can have it and not know until you’re unable to get pregnant.
Advertisement
There’s no connection between your symptoms and the severity of the condition. Some people may have very few patches of endometriosis and still experience severe pain. Other people might have many patches of endometriosis, but not experience any pain.
Endometriosis doesn’t cause weight gain, but the bloating and fluid retention can make you feel like you’re gaining weight.
Healthcare providers don’t know for sure what causes endometriosis. When you have endometriosis, tissue that is similar to the lining of your uterus grows in the wrong places. Researchers are looking for a connection between endometriosis and conditions like retrograde menstruation, immune system conditions and hormone disorders as possible factors that may lead to the condition.
Although experts don’t know the exact cause of endometriosis, they do see a connection between a family history of the condition and an increased risk of developing it at some point. If another person in your biological family — your mother, grandmother or sister — has endometriosis, talk to your healthcare provider about your risk.
Endometriosis is a condition that most commonly impacts females between the ages of 20 and 40. It can also happen to younger people during their teenage years. Although many people find relief from endometriosis symptoms after menopause, it can still cause discomfort and pain.
Some factors can place you at a higher risk of developing endometriosis, including:
There are several complications that can happen if you have endometriosis. It can cause pain that disrupts your well-being and daily life. People with endometriosis may also experience fertility issues.
Other than chronic pain and infertility, severe endometriosis can lead to complications like:
Your healthcare provider will work with you to manage these issues to improve your daily life.
Endometriosis is one of the leading causes of infertility. Endometriosis causes tissue to grow in places where it doesn’t belong. This can interfere with how a sperm and egg move to meet each other at conception.
Advertisement
In many cases, an endometriosis diagnosis will start with your symptoms. Painful and heavy periods might cause you to reach out to a healthcare provider. At your appointment, the provider (a gynecologist) may start by asking you for your medical history and if any other people in your biological family have endometriosis. They’ll perform a pelvic exam. Then, they may order imaging tests like an ultrasound or MRI.
The only way to definitively diagnose endometriosis is with a laparoscopy. This procedure involves your healthcare provider using a small camera (laparoscope) to look inside your pelvis. Once they see where the tissue is, they can remove a sample of tissue (biopsy) and send it to a lab for testing.
The surgeon will also try to remove or destroy all tissue that is suspicious of endometriosis that they find during this procedure. In this way, a laparoscopy helps with diagnosis and treatment. Sometimes, the location of endometriotic lesions may make it hard to remove without damaging the underlying critical structures. This operation may require an intervention from a team of surgeons such as minimally invasive gynecologists, colorectal surgeons or urologists.
Sometimes, you find endometriosis by accident. Not all people who have endometriosis will experience symptoms. In these cases, your provider might discover the condition during a different procedure.
Advertisement
Your healthcare provider will help create a treatment plan for endometriosis based on a few factors, including:
In many cases, your treatment plan will focus primarily on managing your pain and improving fertility issues (if you’re planning on a future pregnancy). Medication and surgery (or both) are possible treatment options.
Medications can help manage the symptoms of endometriosis. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can be helpful with pain. Hormonal therapies are another option. They can help with pain and with suppressing your menstrual cycle.
Hormonal options for endometriosis can include:
Advertisement
With all of these medications, it’s important to note that your symptoms can come back if you stop taking the medication. Providers don’t recommend these medications during pregnancy or if you’re actively attempting to achieve pregnancy. Talk to your healthcare provider about the pros and cons of each medication before starting.
In some cases, your provider might recommend surgery to treat endometriosis. There are always risks to a surgical procedure. But surgery for endometriosis can be an effective way to relieve pain and, in some cases, improve your fertility. The goal of surgery is to remove the endometriosis tissue.
Surgical options to treat endometriosis include:
Endometriosis is a chronic disease. Many people experience relief from endometriosis pain after surgery, but the symptoms may return within a few years. The severity of your endometriosis could play a part in how quickly — if at all — it comes back after surgery. Your provider might suggest combining a surgical procedure with medications for the best outcome.
In some cases, endometriosis can go away on its own. This can also happen after menopause, which is often related to a drop in the amount of estrogen in your body.
Many people need to continuously treat endometriosis to manage symptoms like pain. It’s important to maintain a regular appointment schedule with your healthcare provider so you can work together on managing your condition long term.
Over time, the endometrial-like tissue that grows outside of your uterus can cause cysts, adhesions and scar tissue. This can cause you to experience long-term, severe pain, especially during your period. Many people with endometriosis also have difficulties getting pregnant.
Endometriosis can impact your life in many ways — physically and emotionally. While the symptoms can be worse for some and easier for others, the condition is bound to create challenges for you.
You may be in a battle with constant pain — pain that prevents you from enjoying your life or having sex with your partner. The emotional side effects can be just as painful, but in a different way. You may have planned for a child but now have to put those plans on hold as you navigate infertility. Even if pregnancy isn’t on your radar and your pain is manageable, you may have to take medication daily or have surgery to treat endometriosis.
No matter your situation, the good news is that there are treatment options available. With treatment, many people find relief from the symptoms of endometriosis.
Yes, you can get pregnant. But it may be more challenging for you compared to people who don’t have endometriosis. If you have endometriosis and want to get pregnant, talk to your healthcare provider about the best treatment option for you. You might need to have surgery to treat endometriosis. Your provider will work with you to find the best treatment plan to help support pregnancy.
It isn’t typical to develop endometriosis after menopause. If you have it after menopause, it may be because you had it before menopause and it may have reactivated due to taking hormone replacement therapy (HRT).
Endometriosis isn’t a condition you can prevent. But certain factors can reduce your risk of developing the condition.
Endometriosis seems to occur less likely in people who:
Contact a healthcare provider if you have symptoms of endometriosis like pelvic pain or heavy and long menstrual periods. A provider can examine you and run tests to see if endometriosis may be the cause of your symptoms.
It’s natural to have questions if you have endometriosis. Some questions you may want to ask include:
An endometriosis diagnosis can make you feel several emotions. You may feel relief that you finally have answers to what’s been causing your pain and heavy periods. But you may also be fearful about treatment and worried about preserving your fertility. These feelings are all valid, and you’re not alone. Talk to your healthcare provider about your options and what they recommend based on your situation. Medication and surgery can help treat endometriosis.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Endometriosis symptoms can interrupt your life. At Cleveland Clinic, our experts create a treatment plan that matches your lifestyle and goals.
