Amniotic fluid embolism (AFE) is a dangerous and life-threatening complication that occurs during delivery or shortly after giving birth. Amniotic fluid embolism is very difficult to diagnose because the symptoms can be similar to other serious complications during childbirth. Its exact cause is unknown. AFE is very rare.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
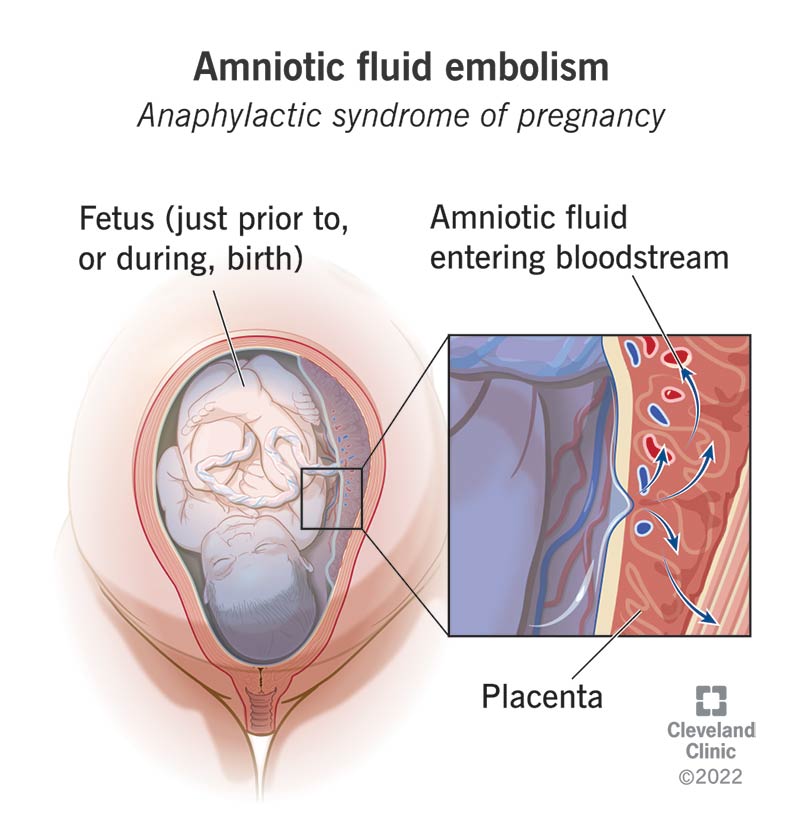
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15463-amniotic-fluid-embolism)
Amniotic fluid embolism (AFE) is a rare and life-threatening complication that occurs when a pregnant woman gets amniotic fluid into their bloodstream just before, during or immediately after childbirth.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Amniotic fluid is the liquid that surrounds the fetus in your uterus during pregnancy. It’s made of mostly water but also contains fetal cells and tissue. For reasons that are mostly unknown, some people have a severe allergic response to amniotic fluid mixing with their blood.
An amniotic fluid embolism can lead to heart and lung failure, which causes several complications due to a lack of oxygenated blood in your body. This could include cardiac arrest (your heart stops beating). People with AFE may also bleed uncontrollably from their uterus or C-section incision.
AFE happens suddenly and is unpredictable. It’s extremely challenging to treat and requires emergency medical care.
Amniotic fluid entering your bloodstream is a normal part of the birthing process. In most people, it doesn’t cause an allergic reaction. Researchers aren’t entirely sure why some people react to amniotic fluid this way while others don’t.
AFE is also known as anaphylactic syndrome of pregnancy.
AFE is rare. It affects 1 in every 40,000 deliveries in the United States and 1 in every 53,800 deliveries in Europe.
The symptoms of AFE are similar to other complications during childbirth, like uterine rupture, placental abruption and eclampsia. This makes it more difficult to diagnose AFE as the cause of the complication.
Advertisement
Risk factors for AFE are hard to predict because it’s rare and hard to study. However, current research points to a few possible risk factors, including:
Signs and symptoms of AFE develop suddenly and quickly. They’re similar to symptoms of other complications during pregnancy and childbirth, making the condition more challenging to detect. Possible symptoms include:
AFE can cause serious complications for you and the fetus. For you, these include:
The fetus is at risk of complications depending on when an amniotic fluid embolism occurs. An emergency delivery may be necessary if symptoms begin before the fetus is born. Babies who are delivered once AFE has already begun are at risk for not getting enough oxygen. Lack of oxygen could cause impairments in their nervous system or brain.
There isn’t a known cause of AFE. The placenta breaking down during labor or delivery may trigger an immune response in some people, leading to AFE. It’s not clear why this happens in some people and not others.
Yes. Amniotic fluid embolism can occur during vaginal and C-section deliveries.
Diagnosing amniotic fluid embolism is difficult because many of the symptoms can overlap with other serious medical conditions. Your provider will rule out other possible causes while working to diagnose amniotic fluid embolism. Amniotic fluid embolism typically occurs in labor or within 30 minutes of delivery. If you have AFE, you’ll need immediate treatment to avoid potentially fatal complications.
Your provider may diagnose AFE if the following symptoms are present:
Advertisement
Healthcare providers classify amniotic fluid embolism into two stages:
Since AFE is a medical emergency, healthcare providers are working quickly and can’t rely on imaging or blood tests for a diagnosis. However, if you survive an amniotic fluid embolism, your provider may order the following tests:
Amniotic fluid embolism is an emergency. Treatment for this condition will need to happen very quickly to protect you and the fetus. Several methods your provider may use include:
Advertisement
Because AFE is difficult to diagnose and dependent on so many factors, it’s challenging to assign a percentage to how many people die from the condition. Studies vary depending on how the data is collected, but the death rate may be as high as 60%.
It depends on how severely you react to AFE as well as your health history. There can be both physical and psychological side effects from amniotic fluid embolism. Some long-term effects could include:
Unfortunately, there’s no way to prevent amniotic fluid embolism. Healthcare providers are still unsure why AFE happens and what exactly causes this condition.
One way to prepare for any kind of medical emergency is to develop a plan with your family and healthcare providers. Ask your healthcare provider about emergency situations and how your medical team approaches these situations.
This may be a part of your birth plan (a document you develop before giving birth with your wishes for the birth). Remember, your birth plan represents the ideal situation. If there is ever an emergency, your healthcare team will need to act accordingly to protect the health of you and the fetus.
Advertisement
Amniotic fluid embolism (AFE) is a life-threatening complication that occurs during labor and delivery. It’s rare and happens suddenly and quickly. AFE is not well-understood and there’s nothing you can do to prevent it from happening. Medical researchers are also unsure why AFE happens to some people and not to others.
If you’re pregnant, your chances of developing AFE is very low. Discuss your concerns about this rare condition with your pregnancy care provider so they can help ease your worries. If you’ve survived AFE, you may have long-term physical or psychological side effects. Talk to your provider, partner or friends so they can support you in your recovery from AFE.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
From routine pelvic exams to high-risk pregnancies, Cleveland Clinic’s Ob/Gyns are here for you at any point in life.
