Immune thrombocytopenia (ITP) is a rare blood disorder that affects how your blood clots. When your blood can’t clot, you may bruise easily, bleed more than normal when you’re hurt or start bleeding for no reason. Sometimes, ITP goes away without treatment. Other times, it’s a chronic condition, meaning treatment eases symptoms but doesn’t cure it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
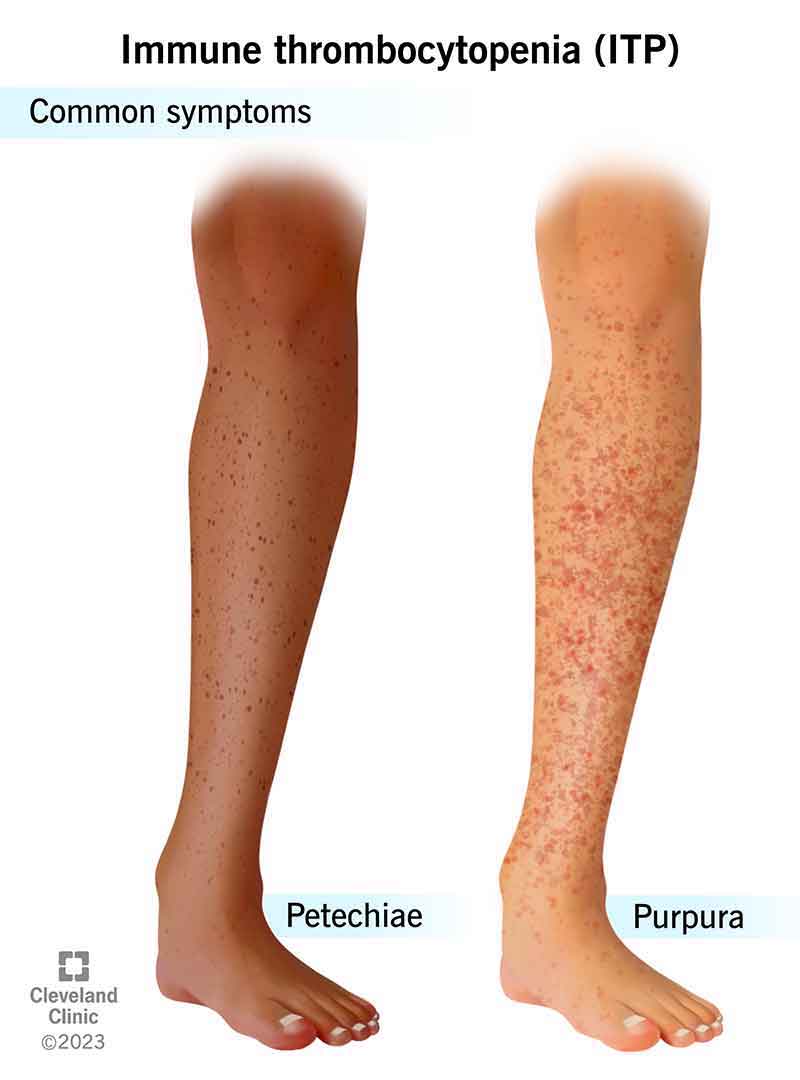
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/5726-immune-thrombocytopenia)
Immune thrombocytopenia (ITP) is a form of low platelet count, a condition that keeps your blood from clotting. When your blood can’t make clots, you may bruise easily, bleed a lot when you’re hurt or start bleeding for no reason. Immune thrombocytopenia happens when your immune system clears your platelets from circulation and your platelet level goes down. In some cases, ITP goes away on its own or with treatment. Other times, immune thrombocytopenia is a chronic condition, which means symptoms can be treated, but not cured. People with chronic ITP may need treatment for the rest of their lives.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It’s rare. Each year, about 4 in 100,000 children and 3 in 100,000 adults in the United States learn they have this condition.
The two ITP types are:
Healthcare providers classify ITP by the amount of time you’ve had the condition:
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_4h5dwvob/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Separating common misconceptions from medical facts about chronic immune thrombocytopenia (ITP).
You may not have any symptoms, but they can happen slowly or quickly if you do. Symptoms may include:
Advertisement
Immune thrombocytopenia happens when your immune system makes antibodies that mistakenly identify your cells as being invaders, and then direct other immune cells to attack your platelets. When something damages or cuts your blood vessels, platelets swarm the damaged area, sticking together to make a blood clot that stops bleeding (primary hemostasis). Experts don’t know what triggers the immune system attacks on platelets.
Research shows people with human immunodeficiency virus (HIV), H. pylori infections or hepatitis C have an increased risk of developing ITP.
Before making a diagnosis, your healthcare provider will do a physical exam to check for bleeding on or under your skin. They’ll ask about your medical history. That’s because ITP symptoms are like other bleeding disorder symptoms. Likewise, ITP may be a complication of blood cancer. Your provider will eliminate other possible causes before making a diagnosis.
Providers may do the following tests:
If you’re at risk for HIV, hepatitis C or H. pylori, your provider may do tests for those infections.
Often, children with immune thrombocytopenia have mild symptoms and don’t need treatment, but most adults will. If you do need treatment, your healthcare provider may prescribe medications to boost your platelet count or keep your immune system from attacking your platelets. Medications may include:
Your provider may recommend other steps like:
Medications, transfusions and surgery may cause several different side effects. Your healthcare provider will discuss treatment side effects, so you know what to expect.
The outlook varies depending on your or your child’s unique situation. If your child has ITP, they’ll probably get better within a few weeks or months without needing treatment. If you have persistent or chronic ITP, you may need medications and other treatments to manage your symptoms depending on how low your platelet count is, but you’ll always have the condition. Healthcare providers can’t cure immune thrombocytopenia, but many people with chronic ITP live for decades with the condition.
Advertisement
If you have ITP, you may need medication for the rest of your life to ensure your body makes enough platelets. And you’ll need to avoid activities that increase the chance you’ll get hurt and start bleeding. For example, you should:
Contact your provider if you notice new bruises or petechia that may be signs that your condition is getting worse. Your provider may do tests to check your platelet levels.
Very rarely, immune thrombocytopenia may make your platelet levels drop so low that you start bleeding uncontrollably. Any bleeding that you can’t stop by applying pressure is a medical emergency and a need to go to the emergency room.
Advertisement
It may help to know that your fetus won’t be affected by ITP. Your baby may have fewer platelets at birth, but their platelet count will increase. If you have a mild case of immune thrombocytopenia during pregnancy, you won’t need treatment. If you do need treatment during pregnancy, your provider will recommend treatments that won’t affect your fetus.
Immune thrombocytopenia (ITP) is a bleeding disorder that keeps your blood from clotting. If you have this condition, you may bruise easily and bleed a lot when you’re hurt. ITP can be scary, particularly if the condition makes you bleed for no reason. Healthcare providers can treat the condition, but they can’t cure it.
If you have ITP, you may need to avoid activities where you might get hurt and bleed. You may need to take certain drugs for the rest of your life and avoid others. Most people with ITP live for decades after their diagnosis. If you have this condition, ask your healthcare provider about ways to live with ITP.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you hear a rare diagnosis like bone marrow failure and cytopenias, you want the best possible care. At Cleveland Clinic we’re experts in these rare conditions.
