Ventricular tachycardia is a fast, abnormal heart rhythm (arrhythmia) that comes from atypical electrical signals in your heart’s lower chambers. These keep normal heartbeat signals from getting through and make your heart beat so fast that it can’t pump enough blood to your body. Treatments include managing the cause and, sometimes, procedures.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
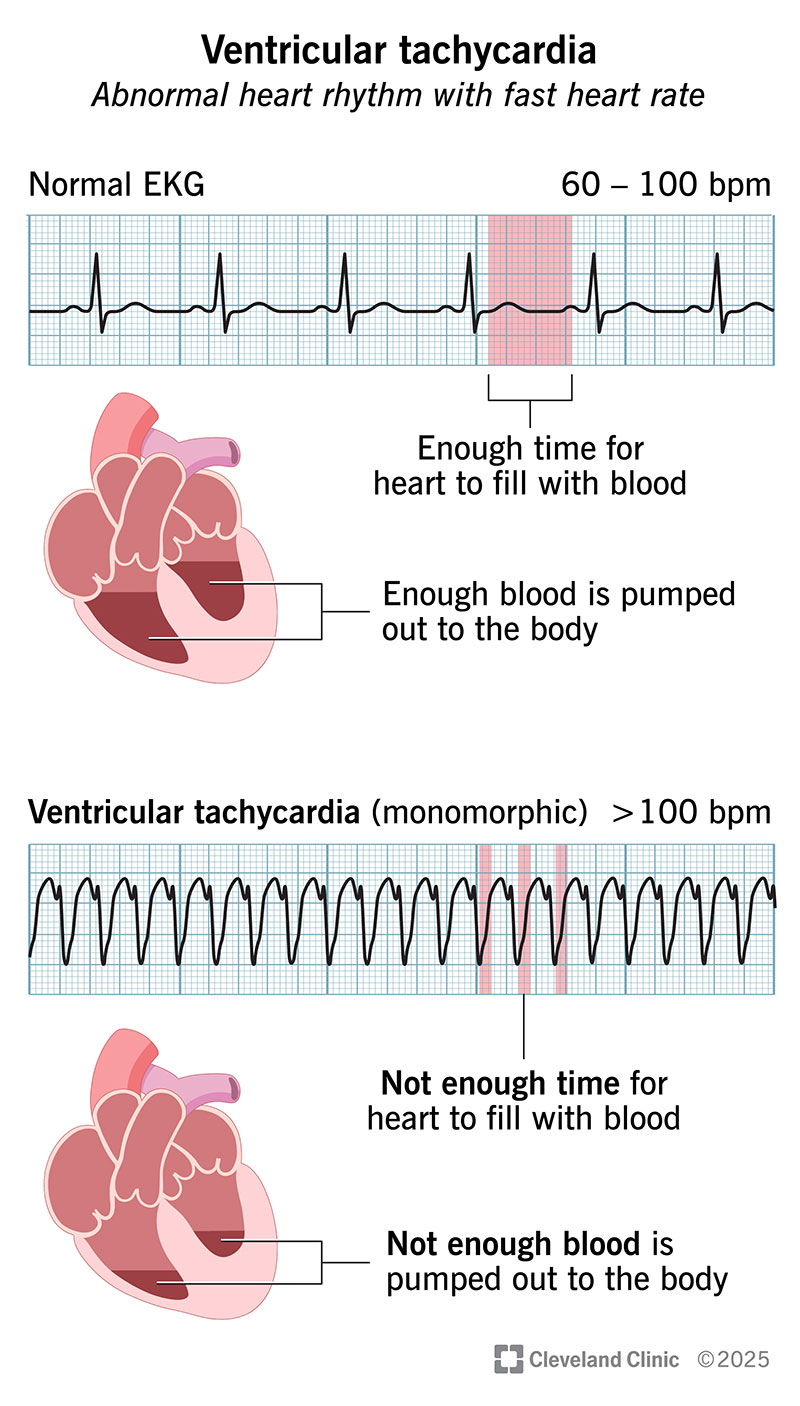
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17616-ventricular-tachycardia-illustration)
Ventricular tachycardia (VT or V-tach) is an abnormal heart rhythm with a fast heart rate of over 100 beats per minute that starts in your heart’s two lower chambers (ventricles) instead of in the normal electrical pathway. This problem can be life-threatening.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Episodes of ventricular tachycardia that last a few seconds may not cause any harm. But if it lasts more than 30 seconds, it’s serious and requires emergent treatment, as it can lead to sudden cardiac death. Sometimes, this rhythm can also change into another dangerous abnormal rhythm called ventricular fibrillation.
When your heart beats in V-tach, your blood pressure drops because your heart can’t pump enough blood and oxygen to your body. You start to have chest pain or dizziness.
This is because your fast heartbeats don’t allow enough time for your heart chambers to fill up before the next beat. Also, the heartbeats aren’t as coordinated and efficient as regular sinus rhythm. It’s like a bus that stops so briefly at a bus stop that it leaves people behind because there isn’t time for everyone to board.
Ventricular tachycardia makes it hard to send blood to your body. Your tissues and cells get oxygen from your blood. Without the oxygen your body needs, you start to have ventricular tachycardia symptoms. These may include:
Many things can cause ventricular tachycardia, but the most common cause is ischemic heart disease (also known as coronary heart disease or coronary artery disease). It means your heart muscle can’t get enough blood and oxygen because of blockages in the coronary arteries. This usually happens because of atherosclerosis.
Advertisement
Sometimes, the cause is unknown. Other causes of V-tach include:
You’re more likely to have ventricular tachycardia if you have a history of heart disease or a family history of certain heart rhythm issues. You may also be more at risk if you have heart failure or issues with your heart muscle or valves. A previous heart attack or heart surgery is also a risk factor. Other things that can increase your chances of V-tach include severe electrolyte abnormalities or the use of stimulant drugs like cocaine.
Avoiding the heart problems that cause V-tach may lower your risk of getting it.
You can protect yourself from coronary artery disease, the most common cause of ventricular tachycardia, in these ways:
The most common test for diagnosing V-tach is an electrocardiogram (ECG/EKG). This records your heart’s electrical activity. Healthcare providers look for three abnormal heartbeats coming from your ventricles in a row if they suspect V-tach. They describe it by how long it lasts and what the waves look like on an EKG.
To diagnose ventricular tachycardia and the cause, your healthcare provider will talk with you about your symptoms, medical history and biological family history. They’ll perform a physical exam that includes checking your pulse. Then, they’ll order tests.
Other tests may include:
You may hear your healthcare provider classify your type of V-tach as:
Advertisement
You need treatment for ventricular tachycardia when you have symptoms or when you have it for more than 30 seconds (with or without symptoms). You may also need treatment if you have short episodes, but they occur frequently — even without symptoms.
Ventricular tachycardia treatment also involves managing (sometimes emergently) any disease that causes the condition. These treatments may improve the abnormal heart rhythm or prevent it from returning. This includes treating heart attacks and coronary artery disease or fixing electrolyte abnormalities.
Nonemergency treatment for ventricular tachycardia usually includes:
Advertisement
In an emergency, V-tach treatment may include CPR (cardiopulmonary resuscitation) and cardioversion, in which a provider uses electrical shocks to try to get your heart back into normal rhythm. You may receive IV drugs like amiodarone or procainamide.
It’s important to keep your appointments for regular follow-ups. Your provider will want to see how you’re doing and make sure your treatment is working. They’ll talk about any symptoms or changes in how you feel.
If you get an ICD, your provider will want to see you one week later and then check your device every three months. They’ll also want to see you each time your ICD sends a shock.
Call 911 or your local emergency number if you have chest pain that lasts more than several minutes, shortness of breath or fainting.
Questions to ask your provider include:
Your prognosis (outlook) depends on how bad your case is and whether you have another heart issue on top of it. The prognosis is worse if your left ventricle doesn’t work well, especially if this is from coronary artery disease. The two-year death rate can reach 1 in 3 for people in this situation who don’t get treatment. An ICD improves survival in this group.
Advertisement
Ventricular tachycardia can go away in some cases. It can last just a few seconds before your heart rhythm goes back to normal. People who have VT from an electrolyte abnormality and no other conditions may have a life expectancy close to a typical one.
For some people, radiofrequency catheter ablation completely cures the abnormal rhythm, and they don’t need another treatment. ICDs, while not a cure, are highly effective at treating life-threatening ventricular tachycardia by restoring normal rhythm so you can live with VT.
Abnormal heart rhythms are unnerving. But being aware of your heart rate and how you’re feeling can help you know when to seek care. Prompt treatment is important for ventricular tachycardia, so don’t delay getting help for yourself or a loved one. Keep taking any medicines your healthcare provider prescribed for you. Be sure to go to all follow-up visits, especially if you received a medical device as part of your treatment. Follow a heart-healthy plan for meals and physical activity that your healthcare team recommends for you.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
