Dry eyes affect the layers of tears that cover your cornea. It happens when you don’t have enough tears or when your tears evaporate too quickly. Symptoms include burning, itching and a gritty feeling in your eye. You may need to try several different treatments to find a solution that works for you.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
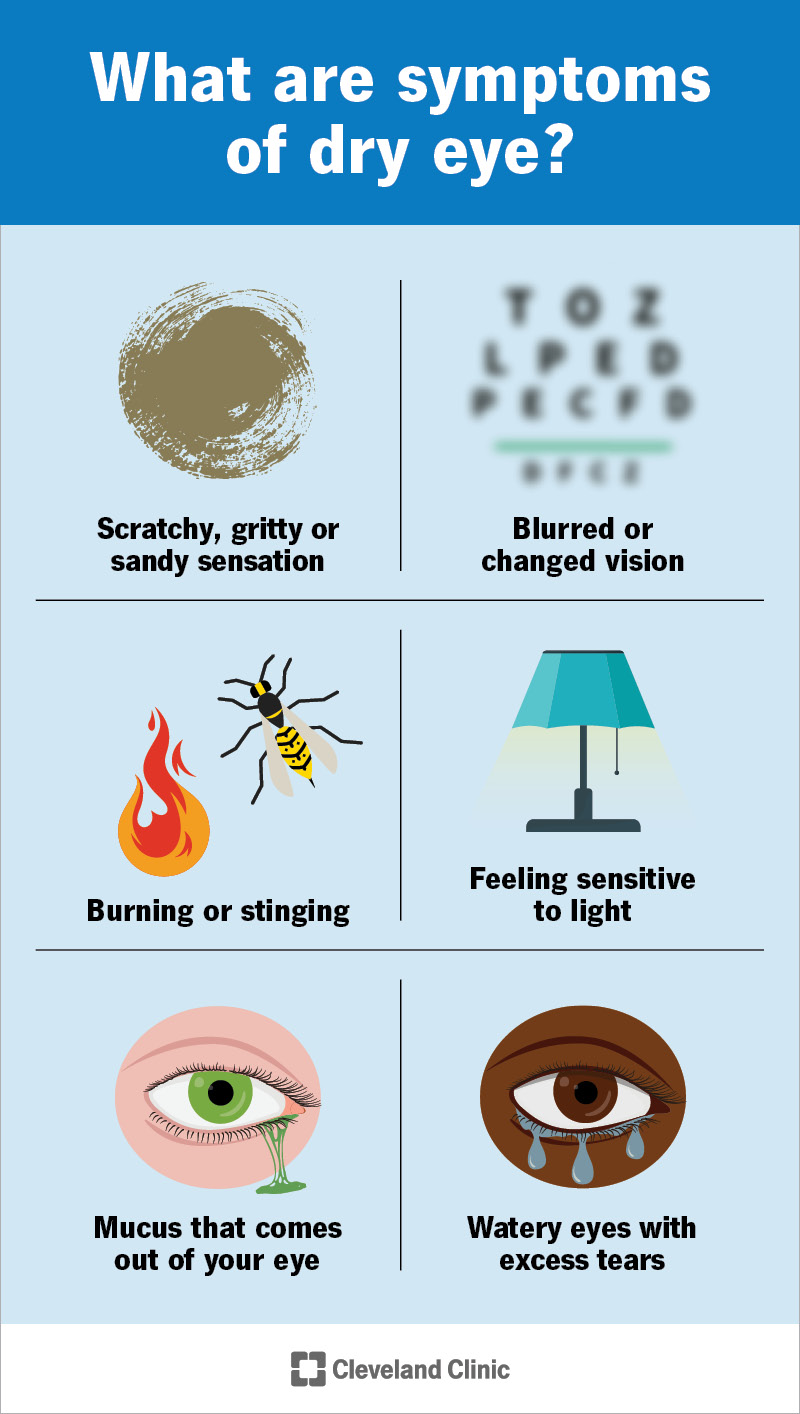
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/dry-eyes-infographic)
Dry eye is a condition that affects your tear film, the three layers of tears that cover and protect the surface of your eyes. You need a smooth and stable tear film to help you see clearly and comfortably. Disruptions to your tear film can cause uncomfortable symptoms, like burning, itching, watering or blurred vision.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Many different factors can prevent your tear film from working as it should and lead to dry eyes. Its causes and risk factors are numerous and complex. So, it may take a while to get to the root of the problem and figure out what’s causing your symptoms. If you have dry eye syndrome, it’s important to establish care with an ophthalmologist or optometrist to manage your condition.
There are a few types of dry eye disease:
When you have dry eye, you may feel like there’s something in your eye that just won’t come out. This can feel like a scratchy, gritty or sandy sensation. Dry eye symptoms may also include:
Advertisement
The symptom of watery eyes may seem confusing. But it’s a very common part of dry eye syndrome. It happens when your meibomian glands aren’t making enough oil. So, the watery layer evaporates too quickly. In response, your lacrimal glands compensate by making too much water. This doesn’t solve the underlying problem.
Causes of dry eyes include:
Eye dryness may occur on its own or along with other medical conditions. In some cases, dry eye is a sign of:
Some risks you can’t control. For example, the older you get, the more likely you are to develop dry eye. But other risks you may be able to manage through lifestyle changes or adjustments to your medications. Risk factors for dry eyes include:
Complications of dry eyes can range from mild to severe. These may include:
Your healthcare provider may ask you to fill out a questionnaire to learn about your symptoms and medical history. You should be prepared to provide lots of information, including:
Then, your provider will give you a thorough eye exam to assess the quality of your eyes and determine what’s causing your symptoms. During your exam, your provider will look for signs of dry eye disease and check the health of your tear film.
There’s no single test that diagnoses dry eye syndrome. Rather, your healthcare provider may use many tests, including:
Advertisement
Your provider may also order other tests, like antibody tests, to check for underlying conditions that could be causing eye dryness.
Dry eye treatment depends on the severity of your symptoms and any underlying conditions you have. You may need to try many different treatments before finding dry eye relief. Treatment for dry eye may include:
Advertisement
Your healthcare provider may suggest you start with home remedies, especially if your symptoms are mild.
Your ophthalmologist will tell you how often you need to come in for appointments. If other medical conditions are causing your dry eye, you may need regular follow-ups with other healthcare providers, too. Be sure to go to all of your appointments so your care team can monitor your condition and help you receive treatment.
Advertisement
Call your ophthalmologist if you experience:
Dry eye is a long-term (chronic) condition. It doesn’t have a cure, but treatments can help manage your symptoms.
You may have to try several different treatments to find what works best for you. This can be a stressful process, but it’s worth the effort. Talk to your provider if your current treatments aren’t working or you want to discuss other options.
Dry eye disease can affect much more than the comfort of your eyes. It can affect your ability to work, socialize and enjoy life. Dry eye can take a toll on your emotions and your mental health, too. You may feel isolated, but you’re not alone. Connect with others who have this condition, and share your experiences. It takes patience and perseverance, but it’s definitely possible to find relief.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic’s ophthalmologists and optometrists have the highest training available. We provide exams, vision correction and care for many eye conditions.
