A cardiac PET scan is an accurate, noninvasive test that creates images of your heart. A healthcare provider can use these images to make decisions about the next steps in your heart care. They can judge how healthy your heart muscle is and decide how to treat it. A cardiac PET scan uses a small amount of radiation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
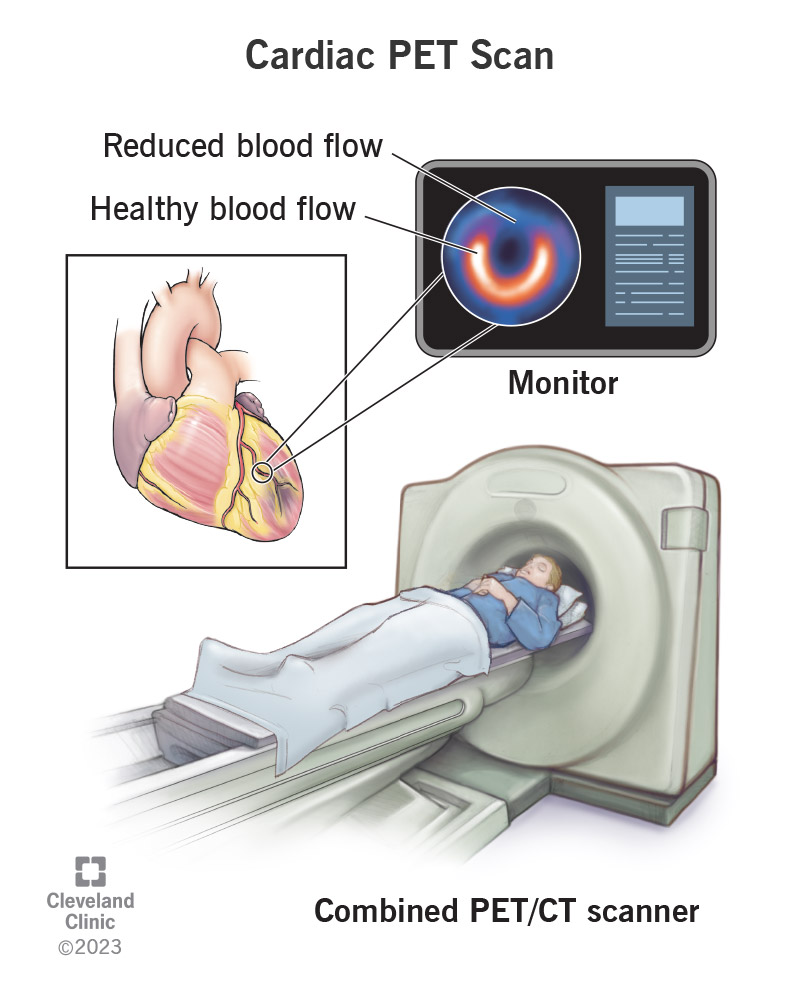
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17376-cardiac-pet-scan)
A cardiac PET (positron emission tomography) scan creates images of your heart using a scanning machine and an injection of radioactive tracers. The test’s radioactive tracers release energy. Depending on the specific type of tracer and the conditions under which a healthcare provider injects it, the pattern with which the tracer lights up your heart can give providers information about how healthy your heart is.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A PET scan of your heart is a noninvasive, accurate test that creates images of your heart from every angle. By looking at what your body’s cells are doing, a cardiac PET scan can provide information other imaging tests can’t. And it can find problems earlier than other tests can.
A combined PET/CT (computed tomography) scanner can take both types of images one after the other with the same machine.
A provider performs a PET scan of your heart when they need to know:
During the test:
Advertisement
Your healthcare provider will give you specific instructions. Be sure to follow them for the most accurate results. In general, you can expect the following to prepare for your heart PET scan:
Don’t do strenuous exercise for 24 hours before your cardiac PET scan.
Don’t smoke on the day of your cardiac PET scan. Nicotine affects the test results.
Bring a list of all medications and supplements you take, including over-the-counter products you buy without a prescription.
Medications with caffeine: Don’t take any over-the-counter medication that contains caffeine (such as pain relievers and diet pills) for 24 hours before your cardiac PET scan. Talk to your provider if you have questions about other medications that may contain caffeine.
If you have asthma: Your provider will likely tell you not to take theophyllinefor 48 hours before your heart PET scan.Bring your asthma inhaler with you to the test.
If you have diabetes: If you take insulin, ask your provider how much you should take on the day of your cardiac PET scan. You may need to take 50% of your usual morning dose and eat a light meal four hours before the test.
If you take pills to manage your blood sugar, your provider will likely tell you not to take your medication before the test. Bring your diabetes medication with you so you can take it after you finish the test. Don’t take your diabetes medication and skip a meal before your heart PET scan.
If you own a glucose monitor, bring it with you to check your blood sugar levels before and after your test. If you think your blood sugar is low, tell your provider right away. Plan to eat and take your medication after your heart PET scan.
If you take heart medications: Ask your provider about changes you need to make to your medications before your cardiac PET scan. Don’t stop taking any medication unless your provider tells you to. You should only take these medications on the day of the test if you have chest pain:
Advertisement
The appointment will take about one to three hours. However, the machine may only scan you for a total of 30 minutes.
After replacing your shirt with a hospital gown and having a blood pressure check, you’ll:
Depending on the disease your provider is checking for, the steps above may differ.
Advertisement
Your healthcare team will ask you how you’re feeling several times during the test. Tell them if you feel:
A provider will remove the IV from your arm or hand at the end of the test. You can change out of your hospital gown and go home. Someone will need to drive you home if you had a sedative.
Be sure to drink a lot of water over the next 24 hours so you can flush the tracer out of your system.
Side effects may include:
Risks for certain people include:
The provider reviewing your heart (cardiac) PET scan can help your referring provider make a diagnosis. Results discuss which areas of your heart muscle may improve with treatment and which may not. Your provider uses this information to decide whether procedures would help your heart pump better. Improving this also improves shortness of breath.
Advertisement
Your provider should receive the results of your cardiac PET scan in 24 to 48 hours. Then, they’ll share them with you, along with any treatment recommendations.
Depending on the condition of your heart muscle, your provider may decide you need:
If these procedures wouldn’t help you because of the extent of heart muscle damage, your provider may recommend that you continue taking medication instead.
Contact your healthcare provider if:
Lying inside a large machine with a small opening can be unsettling, but a cardiac PET scan can provide answers about your heart’s health. This noninvasive, accurate test can provide answers other tests can’t. The sooner you have answers, the sooner you’re on your way to a healthier heart.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
