Mitral valve repair surgery helps people with mitral valve disease live a longer and healthier life. You may need this heart surgery if your mitral valve is very leaky or narrow. Without treatment, these problems can damage your heart over time and even be fatal. Talk with your provider about the treatment plan that’s best for you.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
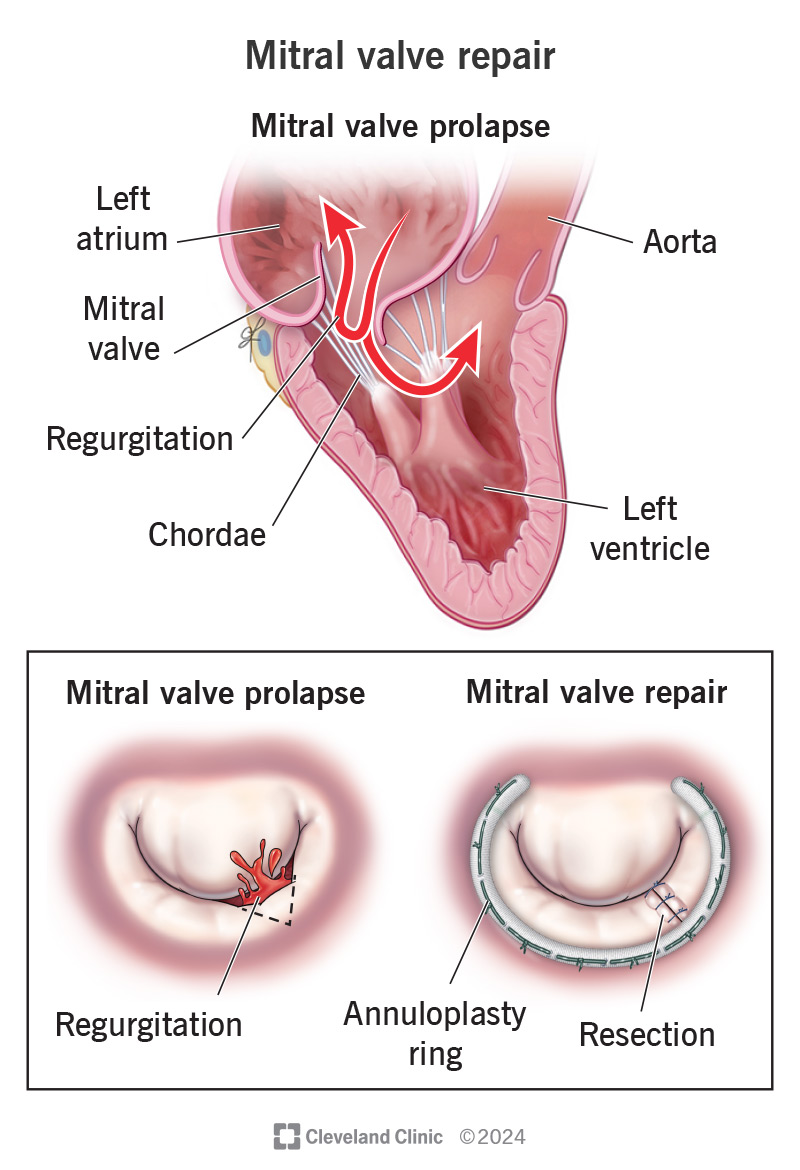
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17240-mitral-valve-repair)
Mitral valve repair is open-heart surgery that fixes problems with your mitral valve. This is the “door” that connects your heart’s left atrium and left ventricle. Your left atrium receives oxygen-rich blood from your lungs. The blood travels through your mitral valve to enter your left ventricle. Then, your left ventricle pumps it out to the rest of your body through your aorta.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Mitral valve disease makes it harder for your valve to do its job. Over time, this can lead to heart and lung damage. A repair can help you avoid or delay this.
If you have severe mitral valve disease, your provider may recommend open-heart surgery to repair or replace your damaged valve. They often prefer repair over replacement — especially when the valve leaks. This is because keeping your own valve offers more benefits and fewer risks.
If you need to have mitral valve repair, it’s important to learn why you need this surgery and what you can expect. Like all heart surgeries, mitral valve repair surgery has risks. But advances in technology continue to make this surgery safer and more effective.
Mitral valve repair treats the following conditions:
Advertisement
People who have mitral valve disease, particularly if the valve leaks, may need mitral valve repair surgery. You also may need surgery if your left ventricle isn’t pumping out enough blood to your body (left-sided heart failure) or your heart is enlarged.
If you have a mild form of the disease, you may not need surgery. Your provider may prescribe medications to manage your symptoms. But they’ll keep a close eye on your valve by using echocardiogram tests to check your heart regularly. You may need surgery later on to manage valve disease that’s getting worse or damaging your heart.
You’ll work with your provider and care team to prepare for your surgery. Be sure to follow your provider’s instructions. Your provider may tell you to:
During mitral valve repair, your surgeon will fix one or more issues with your valve. In general, your surgery will follow these steps. Your provider will:
Providers use several different techniques for mitral valve repair surgery. Talk with your provider about what you can expect for your surgery.
Your surgeon has different options for making an incision, like making:
Advertisement
Almost all mitral valve repairs include an annuloplasty. This means your surgeon places a complete or partial ring around the rim of your valve. The ring may be flexible or rigid. An annuloplasty makes your repair last for a long time.
This is the technique surgeons use most often for posterior leaflet prolapse. Your posterior (back) leaflet and anterior (front) leaflet are the two flaps that make up your valve.
Your surgeon resects (removes) the damaged part of your leaflet and then sews the remaining edges together. Usually, surgeons can make a small, triangular cut to remove the damaged part. But if a larger area of your leaflet is diseased, your surgeon may need to make a rectangular cut to remove more tissue.
Surgeons use this technique to repair both posterior and anterior leaflet prolapse. It involves replacing some of your chordae (chords), which are the tough, fibrous strings that support your mitral valve. Your surgeon removes the ruptured or elongated (too stretched out) chords. Then, they create and attach new chords.
Your surgeon may create new chords out of a tough, synthetic material called Gore-Tex®. Or your surgeon may take healthy chords from another area of your valve and put them in place of the damaged ones. This is called chordal transposition or chordal transfer. Both options provide excellent long-term results.
Advertisement
If you have many calcium deposits on your valve leaflets or annulus, your surgeon will separate your leaflet from your annulus and remove the calcium deposits. Then, they’ll rebuild the damaged part of your valve using a patch or sutures.
After your surgery, you can expect to:
Most people need to recover in the hospital for about a week after surgery to repair their mitral valve.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_1pyvi2ee/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
A. Marc Gillinov, MD, explains the benefits of mitral valve repair.
Mitral valve repair has several advantages over valve replacement. These include:
Whenever possible, your provider will recommend a repair instead of a replacement. Repair is the better option for most people with mitral valve regurgitation.
But replacement surgery is a better option in some situations. It doesn’t take as long as repair surgery, and it’s less complex to perform.
Advertisement
Some people are candidates for procedures other than standard open-heart surgery. These include minimally invasive mitral valve repair and percutaneous interventions. Talk with your provider to see if one of these procedures makes sense for you. Your provider will consider many factors like your age and overall health condition to decide the valve repair method that’s best for you.
Mitral valve repair is successful in most cases. Reports have shown that 10 years later, nearly 94% of people don’t have significant mitral valve regurgitation.
Complications of valve surgery include:
Talk with your provider about all possible complications and how to lower your risk.
Recovery from mitral valve repair surgery usually takes four to eight weeks. Some people may need longer.
You’re probably wondering what life will be like after your mitral valve repair. You know you’ll need to spend some time in the hospital, and you might be planning on cardiac rehab. But what comes next?
The short answer is that recovery looks different for everyone. Your neighbor might’ve bounced back quickly and felt as good as new a month later. But maybe an old friend told you she didn’t feel back to normal for many months. And even then, it felt like a “new normal.”
If it takes you longer, it’s OK. Don’t compare your recovery to what others experience, and don’t push yourself to feel better right away.
Several factors impact your recovery. These include:
After you’re home from the hospital, set small and manageable goals. Get enough rest as you slowly return to your normal routine. You’ll have some limitations after mitral valve repair while you recover.
Your provider will tell you when it’s safe for you to:
You’ll need an echocardiogram each year so your provider can check on your valve function. You may also need antibiotics before certain procedures to prevent endocarditis (an infection of your valve).
Mitral valve repair is a durable solution for treating mitral valve disease. Most people (95%) can go at least 10 years without needing another surgery. Almost as many (90%) can go 20 years. Most people don’t need another mitral valve surgery after a successful repair.
Your life expectancy depends on many factors, including the severity of your mitral valve disease and your overall health. But researchers have found that people who get a repair at the right time have a life expectancy like others of their age and sex.
Mitral valve repair can help you live a longer and healthier life. Like all heart surgeries, it carries risks. Most people survive the surgery. But some people don’t.
The number of people who don’t survive an isolated mitral valve repair procedure is less than 1 in 1,000 at experienced centers.
If your provider recommends surgery to repair your mitral valve, they believe the benefits of the surgery outweigh the risks. It’s important to talk with your provider about your specific risks of having surgery and your chances of survival. Also, ask your provider what you may expect if you don’t have the surgery.
Your provider will let you know how often you need to return for follow-ups. Be sure to keep all your follow-up appointments and tell your provider how you’re feeling. Everyone has some discomfort, and your provider will prescribe pain medication. But call your provider if you have signs of complications. These include:
Your provider will tell you if there are other signs you should look out for. For instance, if you’re taking blood thinners, you should call your provider if you:
It may be hard to know when a symptom is a normal part of recovery, or when it’s a sign of a complication. When in doubt, pick up the phone and call your care team. It’s better to get checked out and learn nothing’s wrong than to ignore a problem that needs medical care.
Yes, a surgeon can perform more than one procedure in one surgery. Many people who have mitral valve disease also have atrial fibrillation (AFib). If you have AFib, your surgeon can perform the maze procedure to treat your AFib during the same operation.
Surgeons also perform the repair for an infection in your valve (endocarditis). Your surgeon will need to remove all infected tissue from your valve. If there’s enough healthy tissue left, your surgeon can reconstruct your valve. Otherwise, you may need a new valve (valve replacement).
Mitral valve repair surgery can give you back the energy and strength you’ve been missing. Like all heart surgeries, it can come with risks. But advances in technology make mitral valve repair safer and more durable with each passing year. Back in the 1920s, when surgeons pioneered mitral valve repair, they used their fingers to open a narrowed valve! We’ve come a long way since then.
Mitral valve surgery is complex. Don’t be afraid to ask your provider many questions so you understand exactly what’ll happen. Also, ask what lifestyle changes you can make after your surgery to support your heart health for years to come.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Problems with your heart can be scary. Our experts can diagnose and treat mitral & tricuspid heart valve disease.
