Mitochondrial diseases are a group of genetic conditions that affect how mitochondria in your cells produce energy. Mitochondria produce most of the energy your body needs. If you have a mitochondrial disease, your cells aren’t able to produce enough energy. There isn’t a cure, but treatment can prevent life-threatening complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
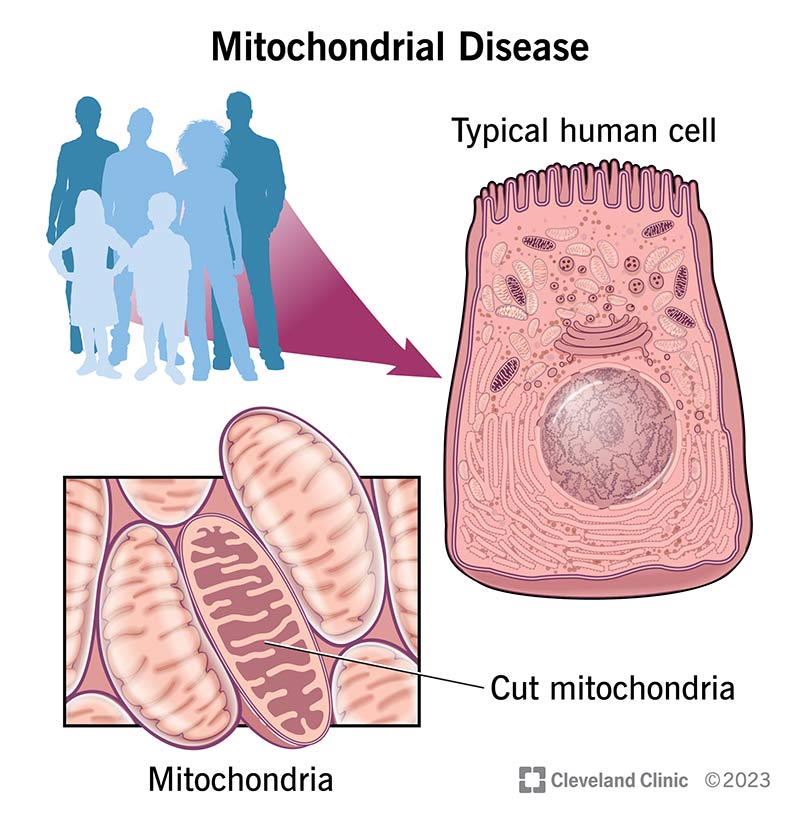
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15612-mitochondrial-disease)
Mitochondrial diseases are a group of conditions that affect how mitochondria work in your body. Mitochondria make energy in your cells. When mitochondria aren’t able to produce enough energy that your body needs, it affects how your organs function.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Mitochondrial diseases can affect almost any part of your body, including the cells of your:
You may hear mitochondria called “the powerhouse of the cell.” Mitochondria are an energy factory. The job of mitochondria is to process oxygen and convert substances from the foods you eat into energy. Mitochondria exist in nearly every cell in the human body. Mitochondria produce 90% of the energy our bodies need to function.
There are many types of mitochondrial diseases. Some of the most common include:
An estimated 1 in 5,000 people has a genetic mitochondrial disease. It’s common for mitochondrial diseases to receive a misdiagnosis due to the number and type of symptoms and organ systems involved, so this number may be underestimated.
Symptoms of mitochondrial diseases vary based on the type and location of the affected cells. They can range from mild to severe and could include:
Advertisement
Symptoms of mitochondrial diseases can be present at birth, but they can also arise at any age. A healthcare provider usually detects symptoms affecting more than one organ or organ system at the same time. Symptoms of the same disease can vary from person to person, even among family members.
A lack of energy production from mitochondria in your cells causes mitochondrial disease. Mitochondria are responsible for producing energy within your body. When your mitochondria don’t receive the instructions they need from your body’s DNA to make energy, it can damage your cells or cause them to die early. This affects how your organs and organ systems function, which leads to symptoms of the condition.
Mitochondrial diseases are genetic. You can inherit these conditions from your biological family in an autosomal dominant or autosomal recessive pattern. This means that you can get a changed (mutated) gene that causes this condition from one or both of your biological parents respectfully. Some cases can occur randomly (de novo) without any history of the condition in your biological family.
Certain cases of mitochondrial disease have a mitochondrial inheritance. This occurs when the mitochondria contain their own DNA. Mitochondrial conditions caused by mutations in the mitochondrial DNA are exclusively inherited from the child's mother.
Yes. Mitochondrial dysfunction occurs when mitochondria don’t work as well as they should due to another disease or condition. Many conditions can lead to secondary mitochondrial dysfunction, including:
If you have secondary mitochondrial dysfunction, you don’t have a genetic mitochondrial disease.
You’re more at risk of developing a mitochondrial disease if it runs in your biological family history or if you have a condition that causes secondary mitochondrial dysfunction. Mitochondrial disease affects both adults and children.
Mitochondrial diseases affect how your organs function. It can cause the following complications:
Complications can be life-threatening.
A healthcare provider will diagnose a mitochondrial disease after a series of examinations and tests that may include:
Advertisement
Other tests, depending on your symptoms and the affected areas of your body, might include:
More advanced testing could include biochemical testing, which looks for changes in body chemicals involved in energy making. A healthcare provider may perform a biopsy where they take a sample of skin and/or muscle tissue to examine it under a microscope.
Yes. Because mitochondrial diseases affect so many different organs and tissues of your body, and you may have many different symptoms, mitochondrial diseases can be difficult to diagnose. There’s no single laboratory test that can diagnose a mitochondrial disease. This is why a referral to a medical facility with physicians who specialize in these diseases is critical to making the diagnosis.
Treatment for a mitochondrial disease varies based on the type and your symptoms. Treatment could include:
Advertisement
There’s no cure for mitochondrial disease. Treatment focuses on preventing life-threatening complications. Treatment that works for one person may differ from what works to treat someone else with the same condition.
Talk to your healthcare provider about side effects before starting treatment. They’ll discuss the side effects of your treatment specifically and what you should look out for. Each type of treatment comes with its own possible side effects.
Your healthcare provider can give you the best advice on your life expectancy after a mitochondrial disease diagnosis. Your outlook depends on your symptoms, affected organs and general health. Some affected children and adults have the same expected lifespan as someone who doesn’t have this condition. Others might experience drastic changes in their health over a very short period of time. Some may have occasional flare-ups of symptoms throughout their lives. Although there’s no cure for mitochondrial diseases, research is ongoing to learn more.
There’s no known way to prevent mitochondrial diseases. If you have a mitochondrial disease, you can avoid situations that can make your symptoms worse like:
Advertisement
A healthcare provider may suggest you conserve (save) your energy to avoid using up all of your body’s energy in a short period of time.
Visit a healthcare provider if your mitochondrial disease symptoms affect your ability to go about your day normally. If you have severe symptoms like a seizure or you have trouble breathing, call 911 or your local emergency services number immediately.
Questions you can ask your healthcare provider include:
It can be difficult to learn that you or a loved one has a mitochondrial disease. The condition can target many organ systems that can potentially cause changes to your lifestyle. In addition to the support from your family and friends, your care team will be available to help you navigate this diagnosis and your treatment options. While there aren’t any cures for mitochondrial diseases, treatment can help reduce symptoms or slow the progress of these conditions.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Mitochondrial disease saps your energy and affects your entire body. At Cleveland Clinic, we can help you learn to manage the symptoms of this lifelong condition.
