Head and neck cancer includes several types of cancers that affect your mouth, throat or other parts of your head and neck. The most common symptom is a persistent sore throat. You can reduce your risk by avoiding tobacco, limiting alcohol and getting the HPV vaccine. These cancers are often treatable if caught early, and most are preventable.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_jyqjcxuk/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn the connection between HPV and oral cancer and how it’s treated.
“Head and neck cancer” is a broad category that includes several cancers that start in regions of your head and neck. Most start in squamous cells that make up the moist tissue lining your mouth, throat (pharynx), voice box or nasal cavity. Providers classify them as head and neck squamous cell carcinoma (HNSCC).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If you have head and neck cancer, your oncologist will work with you to determine the best treatment options. The goal is to fight the disease while preserving those parts of your body that help you speak, eat and make facial expressions. The earlier it’s caught and treated, the better your chances of getting rid of the cancer for good.
Head and neck cancers include cancers in your mouth, parts of your throat (nasopharynx, oropharynx and hypopharynx) and other related structures:
Advertisement
About 4.5% of cancer diagnoses worldwide are head and neck cancers. Most head and neck cancers affect males over 50. But this may be because this group is more likely to have risk factors associated with these cancers, like a history of tobacco use.
In the U.S., instances of tobacco-related head and neck cancers have fallen. Head and neck cancers related to HPV (a type of sexually transmitted infection) are on the rise. Alongside this shift, more people getting diagnosed are under 50.
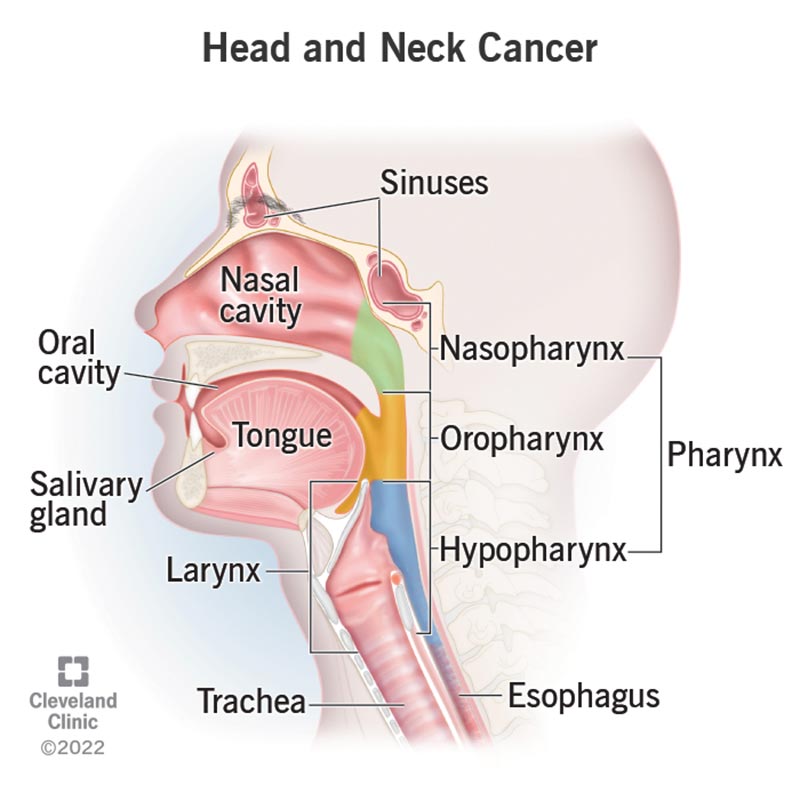
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/14458-head-and-neck-cancer)
Head and neck cancer symptoms are often mild. They can mimic less serious conditions like a cold or sore throat. A sore throat that doesn’t get better is the most common sign of head and neck cancer.
Depending on the type of head and neck cancer, you may experience:
You may notice:
Check with a healthcare provider immediately if you notice any of these symptoms. They may be signs of something less serious, but you’ll need a thorough exam to be sure.
Head and neck cancer starts when a normal cell turns malignant and starts to make copies of itself. The copies form a tumor that can invade tissue and spread throughout your body. Cancer that’s spread is called metastatic cancer.
Researchers have identified several factors that may cause a normal cell to transform into HNSCC.
The most common risk factors for head and neck cancer include:
Advertisement
Other risk factors include:
Diagnosis usually begins with a physical exam. During the exam, your provider will check your mouth, nasal cavities, throat and neck. They may feel your neck, lips, gums and cheeks for lumps.
Advertisement
Based on your provider’s findings, you’ll likely need tests, which may include:
Cancer staging for head and neck cancers helps healthcare providers determine how advanced cancer is. Providers use the TNM (tumor, node, metastasis) system to stage head and neck cancers.
This system considers:
Using this information, your provider will assign a number ranging from I to IV.
The staging specifics differ depending on the type of head and neck cancer. But generally, lower numbers (I and II) mean that the cancer is in the early stages. Early-stage head and neck cancers have the highest treatment success rates.
Advertisement
The main head and neck cancer treatments are:
Your healthcare provider may recommend other treatments, especially if your cancer is advanced or if it went away after treatment but then came back:
Your healthcare provider may also recommend palliative care. Palliative care providers can complement your cancer care by helping you manage symptoms. They can make living with a cancer diagnosis easier, no matter your cancer stage or prognosis.
Head and neck cancer treatments can cause side effects. For instance, surgery to remove a large tumor may change your appearance. Some people treated for head and neck cancers have trouble breathing, eating, swallowing or talking afterward.
Ask your healthcare provider about potential side effects, including ways to manage them. For example, reconstructive surgery or prosthetics may help you achieve your desired appearance following treatment. Regular visits with a speech-language pathologist can help with speaking and swallowing difficulties.
Some head and neck cancers are potentially curable. The chance of a cure is best if your healthcare provider finds the cancer early and treats it immediately. Small tumors that haven’t spread are also sometimes curable.
Your outlook depends on many factors, including your cancer type, general health and response to treatment. Ask your healthcare provider about your prognosis based on your unique cancer diagnosis.
The survival rate for people with Stage I (1) or Stage II (2) oral and throat cancer ranges from approximately 70% to 90%. This means that 70% to 90% of people diagnosed with a head and neck cancer at these stages are alive after five years.
But remember, these numbers are general. They don’t account for your cancer type, health or treatment response. They don’t consider the effects of newer treatments on improving the survival rate. Discuss these factors with your healthcare provider to better understand your prognosis.
You can take steps to help prevent most head and neck cancers. To protect yourself:
If you’ve already had cancer, quitting tobacco and alcohol can reduce your risk of cancer returning.
Even if your provider removes your tumor, you’ll still need follow-up care to ensure you receive immediate treatment if the cancer returns. Depending on your treatment, you may need physical therapy or speech therapy afterward.
Follow your provider’s guidance on caring for yourself during recovery, scheduling follow-up visits and recognizing signs that the cancer has returned.
Questions may include:
Many head and neck cancers are treatable with surgery and/or radiation if they’re found early. See a healthcare provider immediately if you experience any symptoms of head and neck cancer, especially if you smoke or use tobacco. Early detection and treatment are the best ways to fight cancer. Ask your healthcare provider about the best treatment options, depending on your health and cancer stage.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Get compassionate head and neck cancer treatment at Cleveland Clinic. Our providers use the latest tools and research to give you the best possible outcome.
