Male breast cancer develops in breast tissue. Your chest contains undeveloped milk ducts and other tissue where cancer can grow. Without treatment, it can spread throughout your body. Symptoms include a firm, painless lump on one side of your chest. Treatment includes surgery, chemotherapy, radiation, hormone therapy and targeted therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
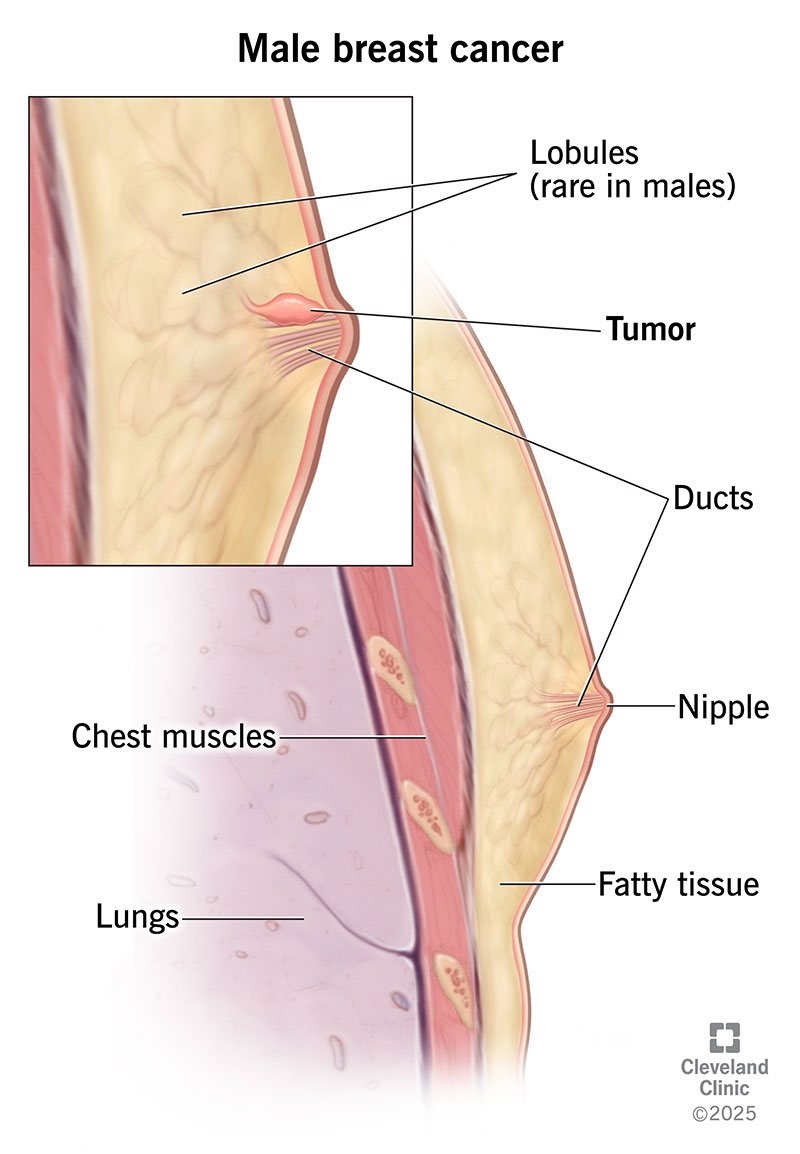
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/9011-male-breast-cancer)
Male breast cancer is a rare form of cancer that grows in the breast tissue in your chest. When most people think of breast cancer, they typically think of women.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
But males also have breast tissue that can become cancerous. One out of every 100 breast cancer diagnoses affects males. About 2,800 males in the U.S. receive this diagnosis each year.
Because it’s so rare, it can be easy to dismiss a lump in your breast as no big deal if you’re male. But it’s important to get all suspicious lumps checked by a healthcare provider.
Cancer is most likely to form in your breast ducts. Ducts are tubes that connect glands called lobules to your nipple. The types of male breast cancer are:
Breast cancer cells can have receptors on them that cause them to grow in response to specific hormones. Think of a receptor as a lock that fits a specific key (hormone). When the hormone attaches to the receptor, cancer cells divide and multiply. Most male breast cancers have receptors that cause cancer cells to grow in response to progesterone and estrogen.
Advertisement
The most common form of breast cancer in males is estrogen receptor-positive (ER+) invasive ductal carcinoma.
The first sign of male breast cancer is often a firm, painless lump in one of your breasts. Usually, it’s behind a nipple. Other signs and symptoms include:
Male breast cancer happens when the DNA inside breast cells changes, or mutates. The mutated cells start multiplying rapidly and don’t die. Eventually, the cancer cells form masses called tumors. Parts of the tumor may break off and spread to other body parts through your lymphatic system or bloodstream. Cancer that’s spread is called metastatic cancer.
Scientists continue to research what causes healthy cells to transform into cancer cells in the first place.
Several risk factors may increase your breast cancer risk, including:
Get genetic testing if you likely have a gene mutation that increases your cancer risk. A family history of breast or ovarian cancer is a clue that the BRCA2 mutation may be in your genes. Not only does it cause breast cancer, but this mutation can also lead to melanoma, pancreatic cancer and prostate cancer.
A healthcare provider can help you decide if you’d benefit from genetic testing.
A healthcare provider will ask about your symptoms and risk factors. Providers perform various tests to diagnose male breast cancer, including:
If the cells are cancerous, pathologists in the lab will check for hormone receptors and the HER2 receptor. (HER2 is a protein that fuels cancer growth.) The results will help your provider plan treatment.
Advertisement
After diagnosing breast cancer, healthcare providers stage it. Staging uses information like tumor size and location to figure out how advanced the disease is. At this point, you may need more imaging tests and a sentinel node biopsy. For this procedure, your provider removes one or more lymph nodes near a tumor and tests them for cancer cells.
The stages of male breast cancer are:
Your treatment depends on the cancer type and stage. You’ll likely need a combination of treatments that follow a timeline that your provider will explain to you.
Breast cancer surgery is the most common treatment for early-stage male breast cancer. Surgery to remove your entire breast (mastectomy) is more common than surgery to remove the lump only (lumpectomy).
Advertisement
A radical mastectomy removes all of your breast tissue. It removes the lymph nodes in your armpit and some chest muscle, too. But it’s more common to get a modified radical mastectomy. This procedure doesn’t remove muscle tissue or as many lymph nodes.
Radiation for breast cancer uses X-rays or other energy sources to kill cancer cells. Radiation usually follows a lumpectomy to kill any remaining cancer cells. It’s possible for surgery to miss small tumor cells close to your chest wall or skin. But radiation can destroy what’s left, so tumors don’t grow back.
Chemotherapy uses drugs to kill cancer cells throughout your body. For local tumors (those that haven’t spread), you may get chemo before surgery to shrink tumors. Or you may need radiation and chemo after surgery to reduce the chance that a tumor will grow back or come back somewhere else in the body. You won’t receive treatments at the same time, but rather one after the other.
Providers use hormone therapy to lower estrogen levels or block their effects. You’ll likely get this treatment if the cancer cells use hormones, like estrogen, to grow. Tamoxifen is a common medication used to treat male breast cancer. Other medicines that keep hormones from fueling cancer growth in males are aromatase inhibitors combined with gonadotropin-releasing hormone (GnRH) agonists.
Advertisement
Targeted therapy treatments interfere with processes that allow cancer cells to grow. Targeted treatments only work on specific types of cancer cells. For example, some treatments only work on breast cancers with hormone receptors. Others, like PARP inhibitors, work on cancer cells with BRCA gene mutations.
See a provider if you have an unexplained lump in your chest that doesn’t go away within two weeks. Follow your healthcare provider’s advice about how often you need cancer screenings.
The biggest factors that affect your prognosis (outlook) are the cancer type and stage. The survival rate is higher for early-stage cancers.
A recent study tracked the mortality (death) rate of males diagnosed with breast cancer based on cancer stage. All had hormone receptor-positive (HR+) breast cancer. Within 20 years of diagnosis, researchers found that:
Unfortunately, many men delay seeing their provider. So, most aren’t diagnosed until the cancer has already advanced. At this point, it’s much harder to treat.
This is why it’s important to seek care if you notice an unexplained breast lump.
Many men don’t think breast cancer can happen to them. So, they may not recognize the signs. But men can and do get breast cancer. This is why it’s vital to see a provider if something isn’t quite right with your chest tissue. Getting diagnosed and treated in the early stages can save your life. If breast cancer runs in your family, talk to a provider about how to detect cancer in the early stages.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s patient-centered care for breast cancer in men includes the latest diagnosis and treatment — with compassionate support at every step.
