Pulmonary nodules are areas of abnormal growth on your lungs. They usually don’t cause symptoms. Providers see them on imaging like X-rays or CT scans. Infections, autoimmune diseases and cancer can cause them. They’re usually noncancerous but your provider may have you get a biopsy or follow-up imaging.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
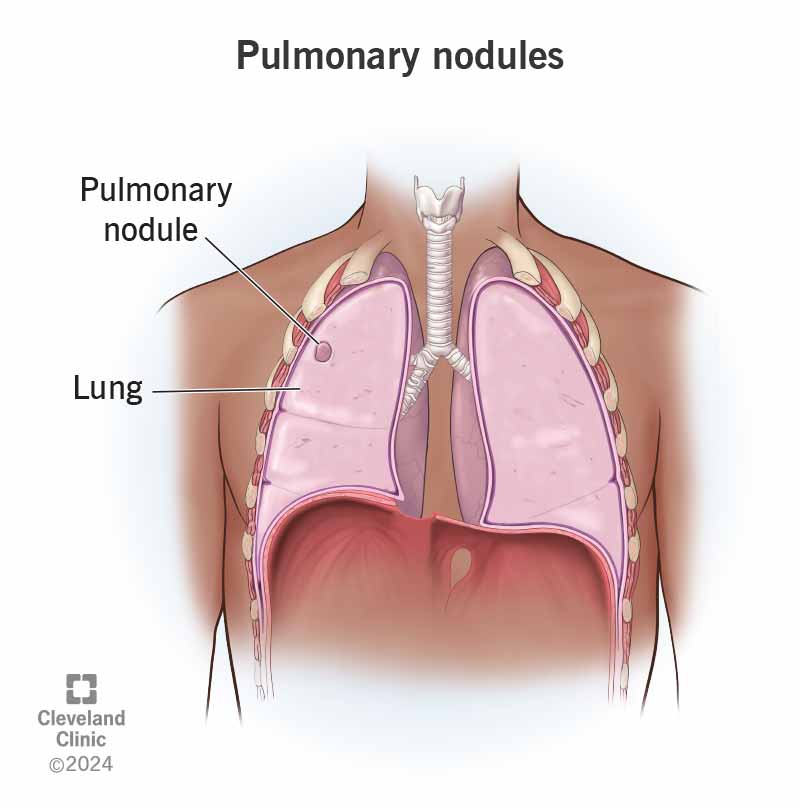
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/pulmonary-nodules)
A pulmonary nodule is a spot on your lung. On chest X-rays or a CT scan these nodules look different from the surrounding (normal) lung tissue.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It can be worrisome to hear that your imaging shows a nodule. But most lung nodules are benign (not cancerous).
You might see providers describe pulmonary nodules by how solid they look on an image. Ground glass opacity means the area is hazy and the provider can still see structures underneath it. Nodules can also be solid (they block the structures underneath them from view) or a mix of both solid and ground-glass opacity.
Pulmonary nodules are common. Radiologists see pulmonary nodules in nearly 1 out of every 3 chest CT scans.
Small lung nodules rarely cause symptoms. If the growth presses against your airway or is cancerous, you might experience:
Infections, inhaled particles, inflammatory conditions, scarring and cancer can all cause pulmonary nodules. Some types of pulmonary nodules and their causes include:
Advertisement
There’s a small possibility that a pulmonary nodule could be cancerous. Rarely, a noncancerous lung nodule may press against or block an airway. You may need surgery to remove the nodule to make breathing easier.
Most people find out they have a lung nodule after getting a screening test or an imaging test for an unrelated reason. If the nodule is suspicious for cancer or you have certain risk factors, your provider might recommend:
No, a provider can’t tell by looking at a CT scan whether a lung nodule is cancerous — only a biopsy can diagnose cancer. But certain features help you provider determine whether you need a biopsy, or if a pulmonary nodule looks benign. For instance, small nodules (smaller than 0.6 centimeters) and those with smooth edges are usually less likely to be cancerous.
Your provider is likely to recommend a biopsy if a nodule is larger than 9 millimeters, or you have certain risk factors for lung cancer. Risk factors include:
Procedures your provider might perform to get a biopsy or surgically remove the entire nodule include:
Small, noncancerous lung nodules don’t usually require treatment. If you have pulmonary nodules caused by an infection, you might need medications to treat the infection. These could include antibiotics or antifungal medications.
Depending on your health history and the size of the nodule, your provider may recommend active surveillance. You’ll get additional imaging in six to 12 months. Nodules that stay the same size during a two-year surveillance period aren’t likely to be cancer.
If the nodule grows or causes symptoms, you may need surgery.
If you have a pulmonary nodule, you might need to follow up with your provider for additional tests or surveillance. Benign nodules will usually stay the same size or even go away on their own. They usually don’t cause symptoms.
Sometimes, a nodule that looks benign can begin to grow. That’s why your provider might recommend monitoring it for changes.
Since most pulmonary nodules aren’t harmful, they don’t affect your survival. If you have a cancerous nodule, the survival rate depends on many factors, including the type of cancer and the stage.
Advertisement
There isn’t much you can do to prevent benign lung nodules. But if you smoke, quitting is the best thing you can do to keep your lungs healthy.
Contact your healthcare provider if you have questions about a finding on an imaging report, like a pulmonary nodule. You may need follow-up testing. Let your provider know if you start experiencing symptoms of a lung condition, like shortness of breath or a chronic cough.
Go to the emergency room or call 911 if you experience:
It might be helpful to ask your healthcare provider:
Finding out you have a pulmonary nodule can be an unwelcome surprise — especially if you’re not having any symptoms. It can be difficult not to worry. But small nodules in people who don’t have risk factors for lung cancer are almost always noncancerous. And for nodules that need treatment, it’s best to catch them before they start causing symptoms. Ask your provider if you have any concerns about pulmonary nodules or any other findings on imaging scans.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Lung nodules are often benign and can be treated or managed. Cleveland Clinic offers personalized lung nodules diagnosis and treatment.
