Hyperthyroidism, also called overactive thyroid, happens when your thyroid makes and releases high levels of thyroid hormone. It speeds up several bodily functions, causing symptoms like rapid heart rate, weight loss, increased appetite and anxiety. Hyperthyroidism is treatable — typically with medications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_fck7e4so/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn the difference between hypothyroidism and hyperthyroidism.
Hyperthyroidism, also called overactive thyroid, is a condition where your thyroid makes and releases high levels of thyroid hormone. It has multiple possible causes. The main thyroid hormones are triiodothyronine (T3), thyroxine (T4) and thyroid stimulating hormone (TSH).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hyperthyroidism speeds up your metabolism, which can affect several aspects of your health. The condition can throw your whole well-being off balance. You may not feel like yourself or even feel out of control of your body. It’s important to get medical treatment if you develop signs of hyperthyroidism so you can get back to feeling like yourself.
Hyperthyroidism is relatively rare. Approximately 1.3% of people in the United States have it.
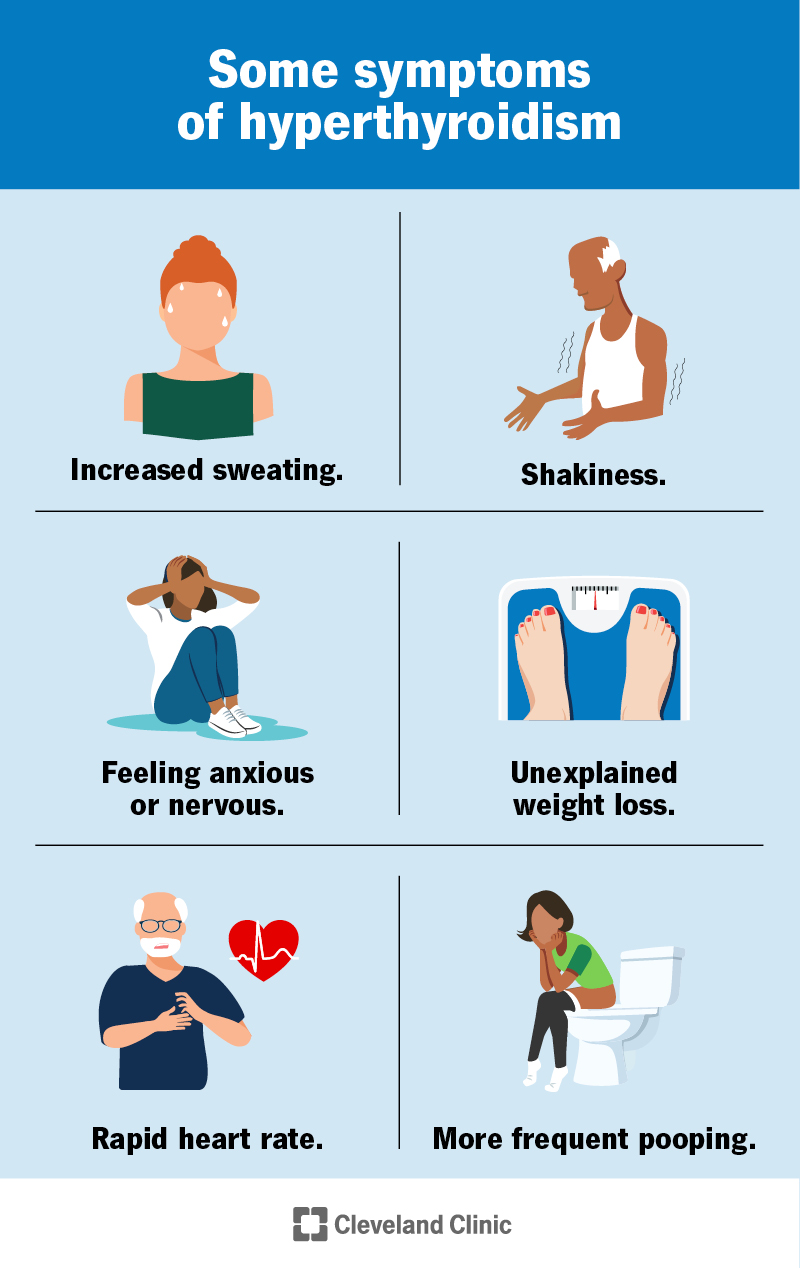
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/14129-hyperthyroidism)
Hyperthyroidism can impact your entire body, so there are many symptoms. You may experience some of these symptoms and not others, or many of them at the same time. Symptoms of hyperthyroidism can include:
These symptoms can start suddenly or develop slowly over time. It’s important to see your healthcare provider if you develop hyperthyroidism symptoms.
Advertisement
Medical conditions and situations that can cause hyperthyroidism include:
Factors that increase your risk of developing hyperthyroidism include:
The diagnostic process for hyperthyroidism may involve multiple steps, including:
There are many treatment options for hyperthyroidism. Depending on the cause, some options may be better for you than others. Your healthcare provider will discuss each option with you and help you determine the best treatment plan.
Advertisement
Methimazole (Tapazole®) and propylthiouracil (PTU) block the ability of your thyroid to make hormones. These medications are the most common treatment for hyperthyroidism. They can usually control thyroid function within two to three months. Your symptoms may get better within days to weeks.
RAI therapy involves taking radioactive iodine by mouth in a single capsule or liquid dose. The radioactive iodine targets your thyroid cells specifically and destroys them. RAI usually leads to permanent destruction of your thyroid, which will cure hyperthyroidism. Most people who receive this treatment must take thyroid hormone medication (levothyroxine) for the rest of their lives to maintain normal thyroid hormone levels.
A surgeon may remove all or part of your thyroid gland through surgery (thyroidectomy). This will correct hyperthyroidism but will usually cause hypothyroidism, requiring lifelong thyroid hormone medication.
Beta-blockers are medications that can help manage hyperthyroidism symptoms like rapid heartbeat, nervousness and shakiness. But they don’t change the level of hormones in your blood. Your provider may recommend beta-blockers alongside another treatment.
Each of these treatments has specific side effects and risks. Your provider will go over them with you. Don’t hesitate to ask questions.
Advertisement
Hyperthyroidism is a treatable condition. Most people do well with treatment. While some forms of treatment require you to take medication for the rest of your life, this will help keep your thyroid hormone levels in a healthy range.
Untreated hyperthyroidism caused by Graves’ disease may get worse over time and cause complications, like Graves’ eye disease (Graves’ ophthalmopathy). If you have Graves’ disease, ask your healthcare provider how you can best manage the condition.
Complications from untreated or undertreated hyperthyroidism include:
A rare and life-threatening complication of hyperthyroidism is thyroid storm (thyroid crisis or thyrotoxic crisis). It happens when your thyroid makes and releases a large amount of thyroid hormone in a short amount of time. It’s an emergency that requires immediate medical attention.
Untreated or inadequately treated hyperthyroidism can cause thyroid storm. Stressors like infection, injury or surgery may trigger it.
If you’re experiencing signs and symptoms of hyperthyroidism, it’s important to see your healthcare provider so they can assess your condition and recommend treatment.
Advertisement
If you already have a diagnosis, you’ll likely need to see your provider regularly to make sure your treatment is working.
If you’re experiencing signs of thyroid storm, like a high fever and very fast heart rate, get to the nearest hospital as soon as possible.
Hyperthyroidism doesn’t typically cause weight gain. In fact, some people experience weight loss — even with an increased appetite. This is because hyperthyroidism speeds up your metabolic rate, causing your body to use more calories for energy than usual.
Hypothyroidism (underactive thyroid) slows down your metabolism, which may lead to weight gain.
During early pregnancy, your body needs to produce more thyroid hormones than normal to help the developing fetus. Having thyroid hormone levels that are a little higher than normal is OK, but if your levels increase dramatically, your healthcare provider may need to form a treatment plan. High levels of thyroid hormones can impact not only you but also the fetus.
It can be difficult to diagnose hyperthyroidism during pregnancy because your thyroid hormone levels naturally increase and the other symptoms of pregnancy can mask signs of the condition.
Eating too many iodine-rich or iodine-fortified foods may cause hyperthyroidism or make it worse in some cases.
If you have hyperthyroidism, your healthcare provider may recommend certain changes to your diet. Always consult your provider or a registered dietitian before making drastic changes to your diet. Know that diet changes alone often can’t fix hyperthyroidism. You’ll likely need medical treatment.
If your provider recommends a low-iodine diet, try to avoid the following foods:
Getting a new diagnosis can be stressful. The good news is that hyperthyroidism is a treatable condition. If you’re experiencing symptoms of hyperthyroidism — like your bodily functions are going too fast — see your healthcare provider. They can have you undergo some simple tests and recommend treatment to get your body back into balance.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s experienced healthcare providers treat all kinds of thyroid disorders, including issues that cause hypothyroidism and hyperthyroidism.
