Depression is a common mental health condition that causes a persistent feeling of sadness and changes in how you think, sleep, eat and act. There are several different types. Depression is treatable — usually with talk therapy, medication or both. Seeking medical help as soon as you have symptoms is essential.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest in things and activities you once enjoyed. It can also cause difficulty with thinking, memory, eating and sleeping.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It’s normal to feel sad about or grieve over difficult life situations, such as losing your job or a divorce. But depression is different in that it persists practically every day for at least two weeks and involves other symptoms than sadness alone.
There are several types of depressive disorders. Clinical depression, or major depressive disorder, is often just called “depression.” It’s the most severe type of depression.
Without treatment, depression can get worse and last longer. In severe cases, it can lead to self-harm or death by suicide. The good news is that treatments can be very effective in improving symptoms.
The American Psychiatric Association’s Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies depressive disorders as the following:
Advertisement
There are also specific forms of major depressive disorder, including:
People with bipolar disorder also experience episodes of depression in addition to manic or hypomanic episodes.
Depression can affect anyone — including children and adults.
Having certain risk factors makes it more likely that you may develop depression. For example, the following conditions are associated with higher rates of depression:
Depression is common. Researchers estimate that nearly 7% of adults in the United States have depression every year. More than 16% of U.S. adults — around 1 in 6 people — will experience depression at some point in their lifetime.
However, researchers believe that these estimates are lower than reality, as many people don’t seek medical help for symptoms of depression and don’t receive a diagnosis.
Approximately 4.4% of children in the United States have depression.
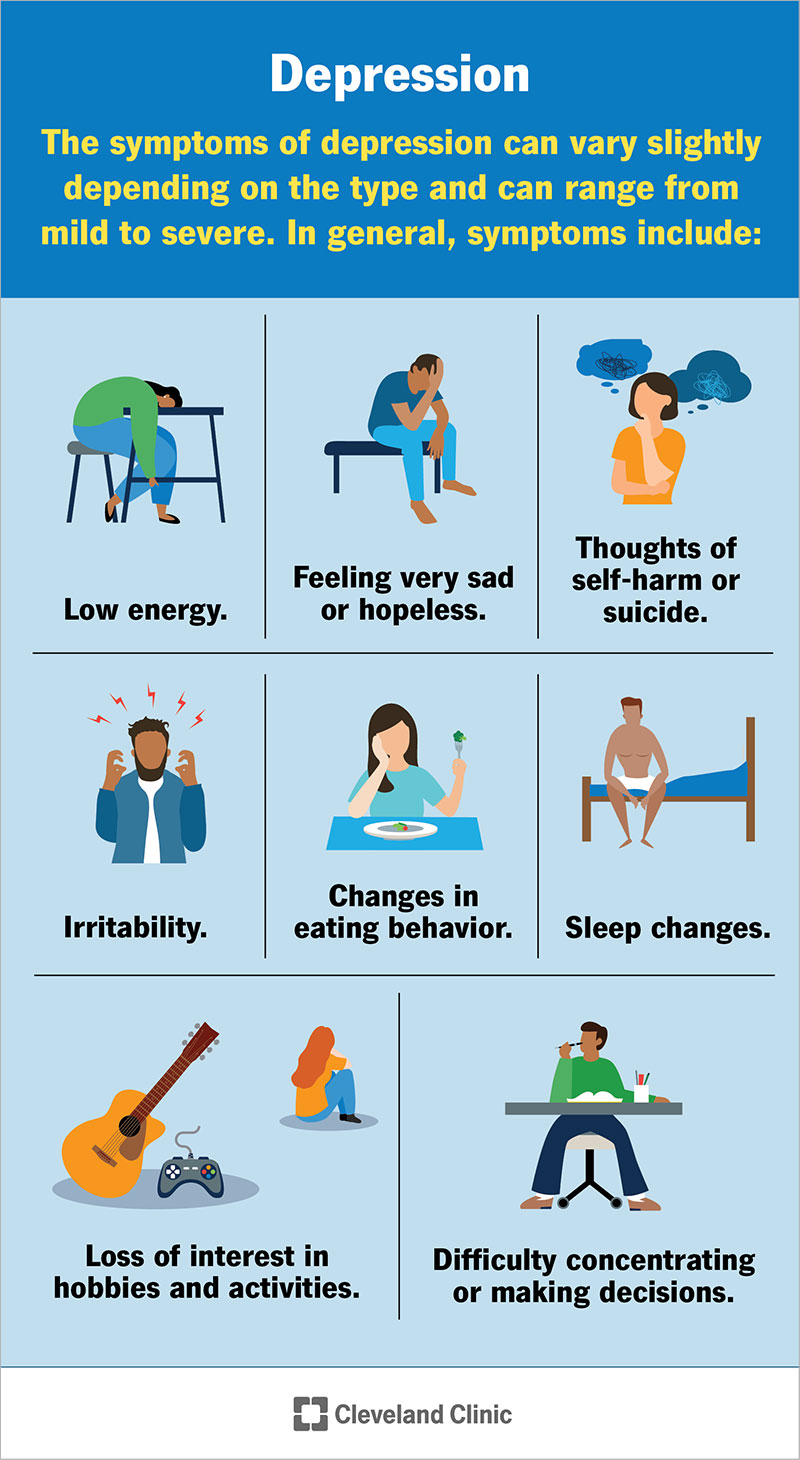
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9290-depression)
The symptoms of depression can vary slightly depending on the type and can range from mild to severe. In general, symptoms include:
Advertisement
If you or a loved one are thinking about suicide, dial 988 on your phone to reach the Suicide and Crisis Lifeline. Someone will be available to help you 24/7.
Researchers don’t know the exact cause of depression. They think that several factors contribute to its development, including:
Healthcare providers diagnose depression based on a thorough understanding of your symptoms, medical history and mental health history. They may diagnose you with a specific type of depression, such as seasonal affective disorder or postpartum depression, based on the context of your symptoms.
Advertisement
To receive a diagnosis of depression, you must have five depression symptoms every day, nearly all day, for at least two weeks.
Your provider may order medical tests, such as blood tests, to see if any underlying medical conditions are causing your depressive symptoms.
Depression is one of the most treatable mental health conditions. Approximately 80% to 90% of people with depression who seek treatment eventually respond well to treatment.
Treatment options include:
Advertisement
There are also things you can do at home to help improve depression symptoms, including:
The prognosis (outlook) of depression varies depending on certain factors, including:
With proper diagnosis and treatment, the vast majority of people with depression live healthy, fulfilling lives. Depression can return after you get treatment, though, so it’s important to seek medical help as soon as symptoms begin again.
Without treatment, depression can:
Depression accounts for nearly 40,000 cases of suicide each year in the United States. It’s essential to get medical help as soon as possible if you’re having suicidal thoughts. Call 911 or 988 (the Suicide and Crisis Lifeline) or go to the emergency room.
You can’t always prevent depression, but you can help reduce your risk by:
If you’ve had depression before, you may be more likely to experience it again. If you have depression symptoms, get help as soon as possible.
If you have symptoms of depression, see a healthcare provider or mental health professional. They can give you an accurate diagnosis and suggest treatment options.
If you’ve started treatment for depression and it isn’t working or you’re having unpleasant side effects, talk to your provider. They can recommend a different treatment plan.
Depression is a common condition that affects millions of people every year. Anyone can experience depression — even if there doesn’t seem to be a reason for it. The good news is that depression is treatable. If you have symptoms of depression, talk to your healthcare provider. The sooner you get help, the sooner you can feel better.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Depression can hamper every aspect of your life. Cleveland Clinic experts are here to help manage your mental health so you can do the things you want.
