Transcranial magnetic stimulation (TMS) is a noninvasive therapy that uses magnetic pulses to change brain activity. It’s FDA-approved for certain mental health conditions. Your provider might suggest it when other treatments don’t help. It’s safe, doesn’t require surgery or sedation, and usually has mild or no side effects.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Transcranial magnetic stimulation is a pain-free, noninvasive treatment that uses magnetic pulses to trigger nerve cells in your brain. It may help manage conditions like depression, obsessive-compulsive disorder and certain types of migraine. Some types of TMS can also help reduce smoking for a short period.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
TMS works by using a small coil placed on your head. It sends magnetic pulses into your brain. These pulses pass through your skull and create tiny electrical signals in your nerve cells underneath. Depending on the pulse pattern, TMS can help wake up underactive areas or calm overactive areas.
If you’ve tried other treatments without much success, your provider may consider TMS as the next step.
There are a few different ways you can get TMS. The main differences are in how the pulses are delivered, how long each session lasts and how deep the stimulation reaches in your brain:
Advertisement
Your provider may recommend different types based on your symptoms and how your brain responds.
TMS may help when other treatments haven’t worked well. In the United States, the FDA cleared different TMS devices and protocols for:
Researchers are also studying TMS to see if it can help with other conditions, like:
TMS can be a helpful option if you haven’t had enough relief from other treatments, like medication or therapy. Many adults with depression or OCD benefit from it. It gives you another choice that doesn’t involve anesthesia or surgery.
TMS isn’t safe for everyone. It may not be a good fit if you have:
Your provider will review your medical history. They’ll talk through any risks to decide whether TMS is right for you.
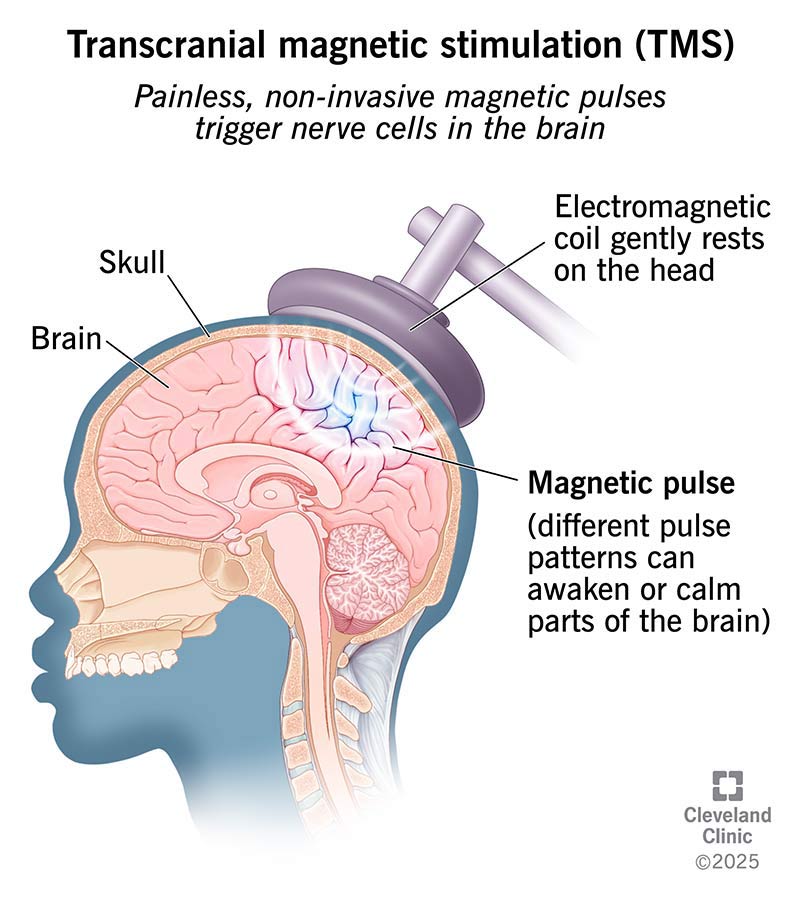
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/transcranial-magnetic-stimulation-tms)
Before treatment, you’ll meet with your healthcare provider for a screening and exam.
Your provider will explain how TMS works and what you can expect during each session. You can eat and drink normally beforehand. And it helps to wear comfortable clothing.
For safety, your provider may recommend that someone drives you to and from your first appointment. Make this plan ahead of time.
Advertisement
The steps might vary slightly depending on the type and clinic where you get treatment. Here’s what you could expect:
Advertisement
Depending on the type of TMS you’re getting, a session can last about three minutes up to around 40 minutes. Accelerated programs may include more than one session in a day.
This treatment may help manage certain mental health conditions, especially when other therapies didn’t offer the right symptom relief.
Here are some possible benefits:
Your provider will help you understand the benefits for your situation.
Most people don’t have side effects. If they do happen, they’re usually mild and improve quickly after each session. TMS doesn’t cause memory loss or problems with thinking.
Advertisement
Common side effects include:
Seizures are the most severe side effect, but they’re very rare. Your provider will check your medical history and watch you during treatment to make sure you’re safe.
After your session, you can go back to your normal day. If you have mild side effects, like a headache, your provider may ask you to rest for a few minutes before leaving. These symptoms usually fade quickly. You might notice condition improvement within a couple of weeks.
TMS usually requires a series of treatments. A common schedule is five days a week for four to six weeks (often about 30 to 36 sessions for depression-related protocols, though this can vary by device and diagnosis). Some accelerated programs deliver multiple short sessions per day over about five days. This can shorten the overall treatment timeline in certain centers.
Your provider will explain the plan that’s right for you. They’ll tell you how many sessions you’ll need and how long your treatment should last. Some people benefit from “maintenance” sessions or an additional short course later if symptoms return.
If you’ve been struggling with a mental health condition and haven’t found relief with other therapies, transcranial magnetic stimulation may be another option. It doesn’t require surgery or anesthesia, and you can return to your day right after a session.
The idea of using magnets on your head might sound a little sci-fi, but TMS is well-studied and FDA-approved. If you’re wondering whether it’s a good fit for you, your provider can explain the benefits, risks and what to expect. Small steps forward may make a big difference in how you feel each day.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
