Non-Hodgkin lymphoma (NHL) is a group of blood cancers that develop in your lymphatic system. They include B-cell lymphomas and T-cell lymphomas. Tumors usually start in your lymph nodes, but they can spread to organs in your lymph system and throughout your body. Some forms of NHL are curable, while others require ongoing treatment or management.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
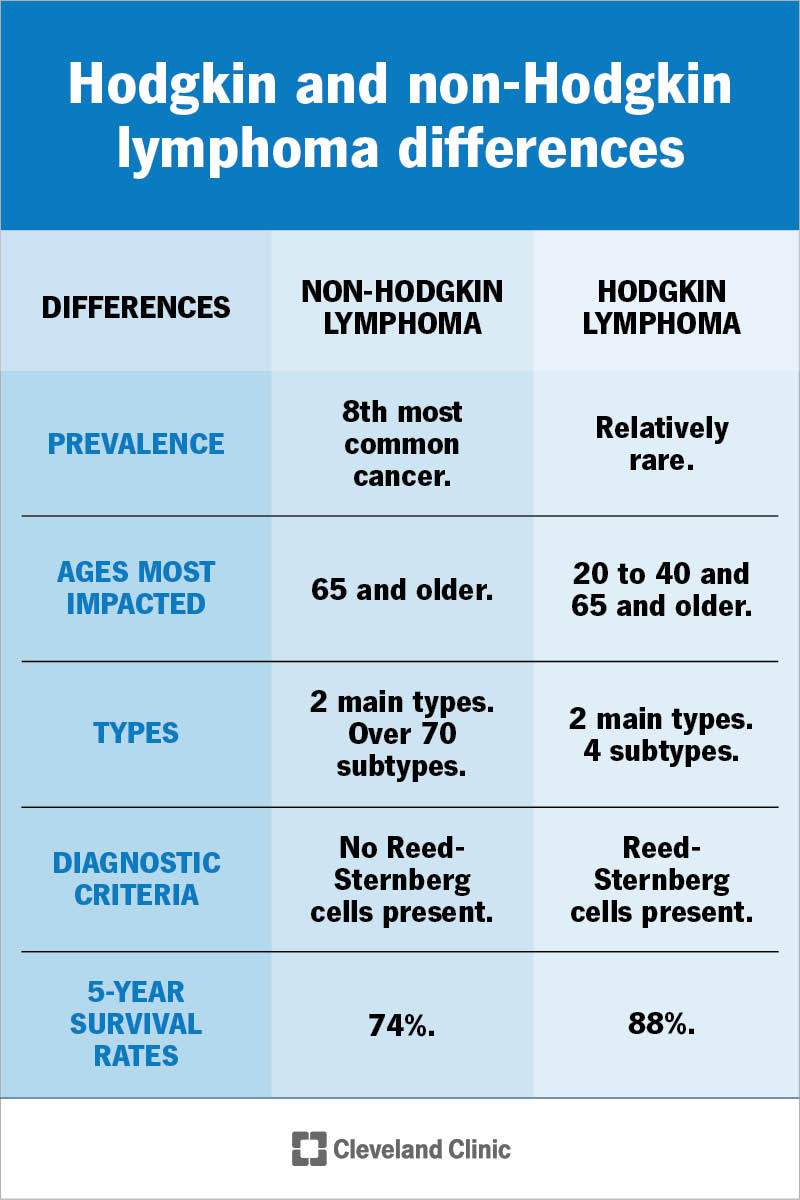
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/hodgkin-non-hodgkin-differences)
Non-Hodgkin lymphoma (NHL) is a group of blood cancers that develop in your lymphatic system. It’s one of two types of lymphoma — cancers that start in white blood cells called lymphocytes. Lymphocytes are important immune system cells that help fight off infections.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With non-Hodgkin lymphoma, genes inside B lymphocytes (B cells) or T lymphocytes (T cells) mutate, or change, at some point in your lifetime. The abnormal lymphoma cells usually form in your lymph nodes and form tumors. But they can also be in other lymph system organs, like your thymus or spleen, or lymph tissue in other places. Without treatment, non-Hodgkin lymphoma can spread.
People with non-Hodgkin lymphoma are living longer than ever, thanks to new treatments. In some cases, treatments cure the condition. Other times, the goal of treatment is to put the disease into remission (no signs or symptoms of cancer) for as long as possible.
There are more than 70 subtypes of non-Hodgkin lymphoma. Healthcare providers classify them based on the type of lymphocyte affected:
Providers classify B-cell and T-cell lymphomas as either aggressive or indolent. Aggressive non-Hodgkin lymphomas spread faster than indolent non-Hodgkin lymphomas. Aggressive NHL often requires more intensive treatment.
Advertisement
They’re relatively common. Non-Hodgkin lymphoma is the 8th most common cancer diagnosis, with 80,620 new cases expected in 2024 in the U.S. It’s the 11th most common cancer worldwide.
Non-Hodgkin lymphoma is much more common than the other type of lymphoma — Hodgkin lymphoma.
The most common symptom is painless swelling in your neck, armpits or groin. This is a sign of swollen lymph nodes in those areas. Other signs and symptoms depend on where the lymphoma cells are. Additional NHL symptoms include:
It’s important to remember that many conditions share these symptoms. Having one or more doesn’t necessarily mean you have non-Hodgkin lymphoma. Still, it’s a good idea to contact a healthcare provider anytime you notice changes in your body that last for several weeks.
Healthcare providers consider whether you have B symptoms when they diagnose lymphomas. B symptoms include fever, night sweats and unexplained weight loss. These help your provider classify the type of non-Hodgkin lymphoma you have and determine the best treatments.
Non-Hodgkin lymphomas form when your body produces too many lymphocytes. These include B cells, T cells or (rarely) natural killer (NK) cells. Acquired genetic mutations that affect lymphocyte growth play a part in the process. “Acquired” means you develop them during your lifetime instead of being born with them.
When lymphocytes mutate, they multiply and eventually become tumors. Usually, the tumors start in your lymph nodes. As your lymphatic system touches nearly every part of your body, non-Hodgkin lymphoma often spreads to other lymph organs.
There are several risk factors linked to non-Hodgkin lymphoma. A risk factor is a trait, activity or condition that increases your risk of developing a disease. For example, people more likely to get diagnosed with NHL are:
Other factors that may increase your risk of NHL include:
Advertisement
A non-Hodgkin lymphoma diagnosis involves many steps. First, you’ll likely need tests to rule out more common conditions that may be causing your symptoms. For example, a swollen lymph node is more likely to mean an infection — not lymphoma. Once your healthcare provider determines you have non-Hodgkin lymphoma, they’ll do tests to determine the type and how advanced it is.
Tests or procedures you may need to diagnose non-Hodgkin lymphoma include:
Advertisement
Test results help providers with cancer staging. Providers stage cancer to develop treatment plans and estimate prognosis, or expected outcome. The stages of non-Hodgkin lymphoma are:
There are several types of treatment for non-Hodgkin lymphoma. The treatment you’ll need depends on factors like the type of NHL, the cancer stage and your overall health. Treatments include:
Advertisement
Common cancer treatments for non-Hodgkin lymphoma — including chemotherapy, radiation therapy and immunotherapy — can cause side effects. Most are short term and go away once treatment ends, while other side effects may be long term.
Ask your healthcare provider about potential side effects before starting treatment. They’ll help you weigh the benefits of treatment against the risks of possible side effects.
In some cases, treatment can cure non-Hodgkin lymphoma. This means that treatment has eliminated all cancer cells for good. This is more common after treatment for aggressive B-cell lymphomas. Most aggressive non-Hodgkin lymphomas that come back usually do so within the first two years after treatment, or they never come back. Still, you’ll need regular check-ups so your healthcare provider can check for relapse.
With other non-Hodgkin lymphomas, especially indolent ones, you may have this condition in the long term. This means you may need continuous or occasional treatment for the rest of your life.
It’s important to remember, though, that even when non-Hodgkin lymphoma isn’t curable, current treatments are helping people live longer, fuller lives with this disease. Most people with indolent lymphoma die from other causes, even if the lymphoma can’t be cured.
According to the U.S. National Cancer Institute, 74% percent of people with non-Hodgkin lymphoma are alive five years after their diagnosis.
Generally, people diagnosed before the condition spreads live longer than people who are diagnosed after cancer spreads. The five-year survival rate for early-stage non-Hodgkin lymphomas (stages I and II) ranges from 79% to 87%. The survival rate for advanced-stage disease (stages III and IV) ranges from 64% to 73%.
You can manage living with non-Hodgkin lymphoma in several ways. These activities won’t make your condition go away, but they may help you feel more confident about living with it:
If you’re receiving treatment for non-Hodgkin lymphoma, you should contact your provider if your symptoms return or get worse. If your treatment has ended, make sure to attend all regular follow-up visits.
Visit the emergency room if you have severe or significantly worsening symptoms that don’t get better despite measures to improve how you feel.
Questions you may want to ask your healthcare provider include:
Learning you have non-Hodgkin lymphoma (NHL) can feel unsettling for so many reasons. After all, there are many types of this disease with different outcomes. Some aggressive types may require more treatment and cause unpleasant side effects — but are ultimately curable. Others may not require treatment right away but will require long-term management. There just aren’t easy answers with this diagnosis.
Your healthcare provider can provide clarity about what your NHL diagnosis means for your health moving forward. In the meantime, know that people diagnosed with this disease are living longer lives. Ask your provider about your prognosis based on your condition.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
There are many types of non-Hodgkin lymphoma. Whether you have an aggressive type or one that’s slow growing, Cleveland Clinic is here with personalized treatment.
