Angioplasty is a procedure that creates more space inside an artery that has plaque built up inside it. Your healthcare provider uses a tiny balloon to force plaque against the artery walls so blood can get through your artery. Often, they also place a stent or tube inside the newly opened space to keep it open.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Angioplasty is a minimally invasive procedure that opens arteries (large blood vessels) to let blood flow more easily. It most commonly treats atherosclerosis (a collection of plaque made of fat and cholesterol) in your arteries.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Angioplasty involves a tiny medical balloon that pushes plaque through in spots that are too narrow or blocked.
Angioplasties are generally safe procedures. They’re less invasive than other heart and vascular procedures, like bypass surgery.
Your cardiovascular health is very important to your overall health. Angioplasties are often necessary to try to prevent serious complications of atherosclerosis, like heart attack and stroke.
Healthcare providers use certain words to explain which arteries they’re treating. The two most common include:
Different angioplasty techniques include:
Advertisement
You may need angioplasty if you have:
Your healthcare provider will use an angiogram (an imaging procedure) to help guide the angioplasty.
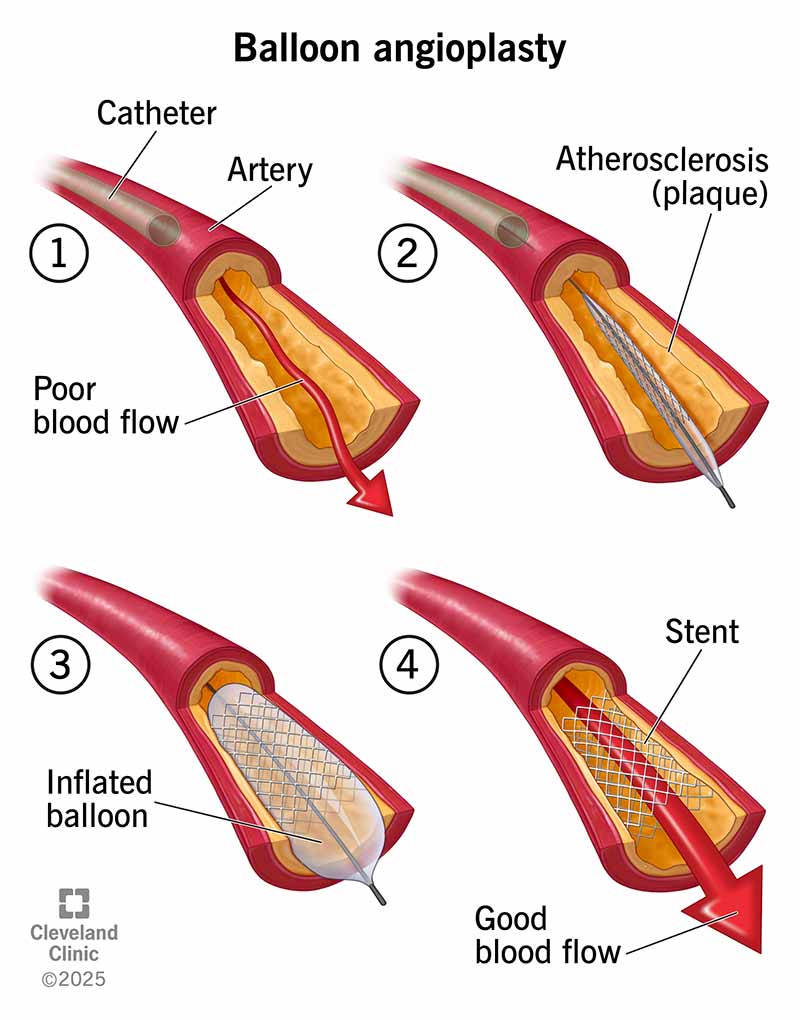
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22060-balloon-angioplasty-with-stent)
Your provider will give you specific instructions for preparing for the procedure. They’ll also go over your medications and health history. In general, your provider will likely:
For your safety, you won’t be allowed to drive yourself home on the same day of the procedure. You should figure out transportation from the hospital if you’re going home the same day. You may need to stay overnight at the hospital.
In general, you can expect the following during angioplasty:
Advertisement
After the procedure, the healthcare provider takes out the catheter. A provider will use a bandage to cover the place where the catheter went into your skin. They’ll put pressure on the site to stop or prevent any bleeding. You may need to lie on your back for a few hours if the catheter was in your groin.
A typical angioplasty procedure can take 30 minutes to two hours. You’ll then need to recover in the hospital afterward. Your healthcare provider can give you a better idea of what to expect for your overall hospital stay.
The risks of angioplasty include:
It’s a good idea to get angioplasty from a healthcare provider who does them often (at a high-volume center). Most of the time, they’re safe procedures. Serious complications are rare.
You’re more likely to have complications if you:
You’ll need to stay at the hospital for several hours or even overnight to recover from angioplasty. If you’re leaving the hospital the same day, someone else needs to drive you home.
Advertisement
You may feel tired after the procedure. Get rest at home and drink fluids. Your provider may tell you to limit your activities for a couple of days after you get home. Your wound may be sensitive or bruised for a week or more.
You may need to take medicines like aspirin or other blood thinners after the angioplasty. If your provider prescribed blood thinners, it’s important to take these as directed. Don’t miss any doses. If you think you need to stop taking them, you should discuss it with your provider before you do.
You should be able to drive and go back to work about a week after the angioplasty. But this can vary depending on the type. Check with your provider.
You’ll have a follow-up visit after you go home. But you should contact your healthcare provider after an angioplasty if:
The success rate of angioplasty varies for several reasons, including:
Your healthcare provider will give you a better idea of what you can expect. Don’t hesitate to ask questions.
Advertisement
Overall, angioplasty should involve minimal pain. You may feel some temporary mild pain or discomfort when the provider:
You shouldn’t feel pain from the catheter during the procedure. You also won’t feel the provider threading the catheter through your blood vessels and arteries.
After the procedure, the sites where the IV and catheter went into your skin may be sore. But this should go away after a week or so.
Tell the provider immediately if you feel intense pain during any part of the procedure.
It can be stressful to hear you need angioplasty. You may be worried about what it means for your health. But angioplasties are often safe and effective procedures. They’re also very common. Don’t hesitate to ask questions if there’s anything you don’t understand. Your provider’s there to help you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
