Rectal prolapse occurs when your rectum, part of your large intestine, slips down inside your anus. It’s caused by a weakening of the muscles that hold it in place. Rectal prolapse may look or feel like hemorrhoids, but unlike hemorrhoids, it doesn’t go away on its own. You'll eventually need surgery to fix it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
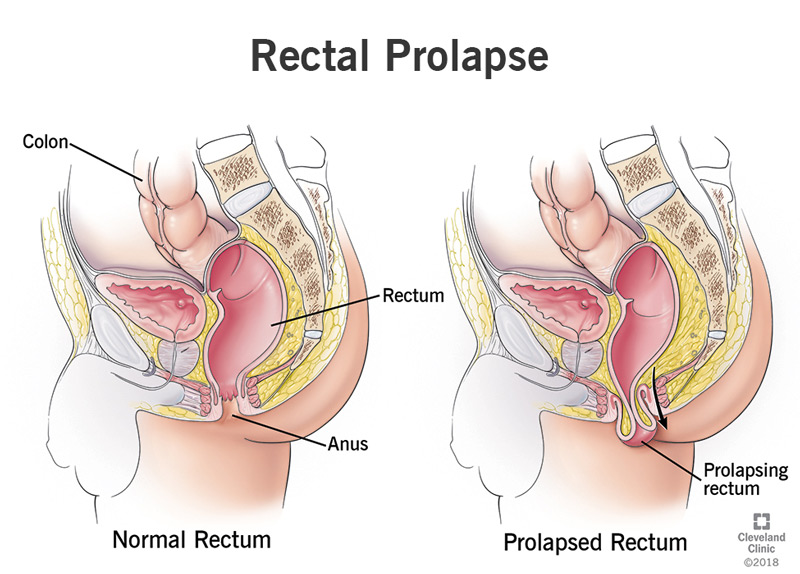
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/14615-rectal-prolapse)
Your rectum is the last segment of your large intestine before your anus. This is where poop prepares to exit your body. When poop arrives in your rectum, it triggers the urge to defecate (poop), and a network of muscles pushes the poop out through your anus. But when rectal prolapse occurs, the rectum itself travels with it, slipping down telescope-style into the anal canal — and sometimes out the other side.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Prolapse” is the term healthcare providers use to describe any body part that has fallen from its normal position in your body. It usually means that the muscles supporting the part have weakened or deteriorated. Some weakening or deterioration is normal with aging, but extra wear and tear on the muscles can accelerate the process. Childbirth, chronic constipation or diarrhea can affect your rectum.
It most commonly affects females, especially those over the age of 50. Less commonly, it may occur in young children as a result of chronic diarrhea or cystic fibrosis.
It’s estimated to occur in about 2.5 in every 1000 people.
It’s not urgently serious, but it can cause discomfort for some people, and it can lead to possible complications down the road. The most common complications are pooping difficulties, such as fecal incontinence.
Failure of the muscles that hold the rectum in place leads to rectal prolapse. Many things may contribute to this. Some possibilities include:
Advertisement
Rectal prolapse can look different in different people. If you have an internal prolapse, your rectum has begun to drop partway into your anus, but it hasn’t yet come out the other end. If you have a mucosal prolapse, the inside mucous lining of your rectum has turned inside-out and begun to poke out of your anus. External prolapse is when your entire rectum falls out. At first, prolapse may only occur when you poop, but eventually, it's constant.
You might notice:
Rectal prolapse and hemorrhoids can have similar symptoms, and it's not uncommon to mistake one for the other. Hemorrhoids — swollen blood vessels in the anus or rectum — can also cause itching, pain or bleeding. Hemorrhoids can even prolapse — slip out of your anus — and they may look similar to mucosal rectal prolapse if they do. After all, they occur within the same red, fleshy mucous lining.
Both hemorrhoids and rectal prolapse can occur during and after pregnancy, or in conjunction with chronic constipation or diarrhea. While rectal prolapse has many possible causes, hemorrhoids are mainly caused by excessive straining. They are also temporary and will go away on their own after a week or so. Rectal prolapse is chronic and progressive. The symptoms may change, but it won’t go away.
Your healthcare provider will review your medical history, then examine your rectum. They might ask you to activate your muscles as if you were pooping. To confirm the diagnosis or rule out other possible problems, they might use one or several of the following tests:
If you have weak pelvic floor muscles, you may have one or several other conditions in addition to rectal prolapse. Your healthcare provider may want to check for these other conditions so that they can address them all together. Possible secondary conditions include:
Advertisement
Not in adults. If rectal prolapse occurs in your child, it might go away after you treat the cause. For example, if your child has hard stools, diarrhea or a parasite infection, treating these conditions will relieve the stress on their pelvic floor muscles. The muscles will repair themselves as your child continues to grow. If you’re an adult, however, rectal prolapse won’t improve without surgery.
If it's not causing bothersome symptoms, you may be able to live for some time with rectal prolapse, taking care of it at home. Taking care of it means pushing your rectum back inside manually. Healthcare providers recommend that you lie on your side with your knees to your chest and use a wet, warm cloth to gently push your rectum back into place. However, prolapse will continue to worsen over time.
Untreated rectal prolapse can lead to several possible complications, including:
Advertisement
There are several surgical approaches to fixing rectal prolapse. Which procedure you have will depend on the specifics of your condition. For generally healthy adults, the first choice is usually a rectopexy, which is a procedure to repair your rectum through your abdomen. However, some people might not be good candidates for abdominal surgery. In these cases, rectal surgery is another option.
This procedure restores your rectum to its original position in your pelvis. Your surgeon will attach your rectum to the back wall of your pelvis (your sacrum) with permanent stitches. They may also reinforce it with mesh. These will hold your rectum in place long enough for scar tissue to develop, which will hold it in place after that. Rectopexy has a 97% long-term success rate in fixing rectal prolapse.
Depending on the judgment and experience of your surgeon, you may have your rectopexy by either open abdominal surgery or minimally invasive (laparoscopic) surgery. Open surgery means opening up your abdominal cavity to access your organs. Laparoscopic surgery is done through small “keyhole” incisions, using a small camera, and is sometimes done with the use of a surgical robot. Both procedures are done under general anesthesia.
Advertisement
If you've had a history of chronic constipation, and if this was a contributing factor to your rectal prolapse, your surgeon may suggest a partial bowel resection at the time of your rectopexy. That means removing a section of your colon. Your surgeon can identify the part of your colon where difficulties with constipation tend to occur. Removing the problem section often improves bowel function afterward.
If abdominal surgery isn’t an ideal option for you, your surgeon may approach your rectal prolapse through your anus. Rectal surgery doesn’t always require general anesthesia as abdominal surgery does. Some people can have it with epidural anesthesia. The rectal or “perineal” approach may also be a better choice if you have a very minor prolapse, or if your rectum is stuck on the outside (incarcerated). There are two common procedures:
Altemeier procedure. In this procedure, your surgeon pulls the prolapsed rectum out through your anus and removes it. They may also remove the lower part of the colon (sigmoid colon) if it is involved in the prolapse (proctosigmoidectomy). Then they sew the two ends of your large intestine (your remaining colon and your anus) back together. The new end of your colon now becomes your new rectum.
This procedure is less invasive than open abdominal surgery and easier to recover from, but its disadvantage is that prolapse may recur afterward. One reason is that the new rectum made from your colon is not as strong as your original rectum was. Because of this, some surgeons combine the altemeier procedure with a “levatoroplasty” — tightening the pelvic floor muscles by sewing them closer together.
Delorme procedure. If you only have a mucosal prolapse, or a small external prolapse, your surgeon may choose a more minor procedure. The Delorme procedure only removes the prolapsed mucosal lining of your rectum. Your surgeon then folds back the muscle wall of the rectum onto itself and stitches it together inside your anal canal. The double muscle wall helps to reinforce the rectum.
All surgeries come with a low risk of certain general complications, including:
Additional risks associated with rectal prolapse surgery include:
It may not be a major problem at first, but it will continue to get worse over time. If you already have bowel problems, you should probably see your healthcare provider sooner than later. Most of the time, surgery will fix rectal prolapse, but it may return in a small number of people. Surgery also has mixed results for bowel complications. These problems may need additional treatment to be solved.
Rectal prolapse is usually the result of a long, gradual process of muscle deterioration. It’s not a medical emergency, but it can be dismaying when it occurs. Some deterioration is inevitable, but self-care can make a difference. By paying attention to your bowel health and exercising your pelvic floor muscles, you can help keep your pelvic organs in the best condition possible. If prolapse does occur, surgery can fix it.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have issues with your digestive system, you need a team of experts you can trust. Our gastroenterology specialists at Cleveland Clinic can help.
