A cystocele occurs when the ligaments and muscles that hold up your bladder stretch or weaken. You may see or feel tissue bulge through your vaginal opening or have difficulty peeing or inserting menstrual products. Sexual intercourse may also be painful. Treatment may include strengthening your pelvic floor muscles or surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
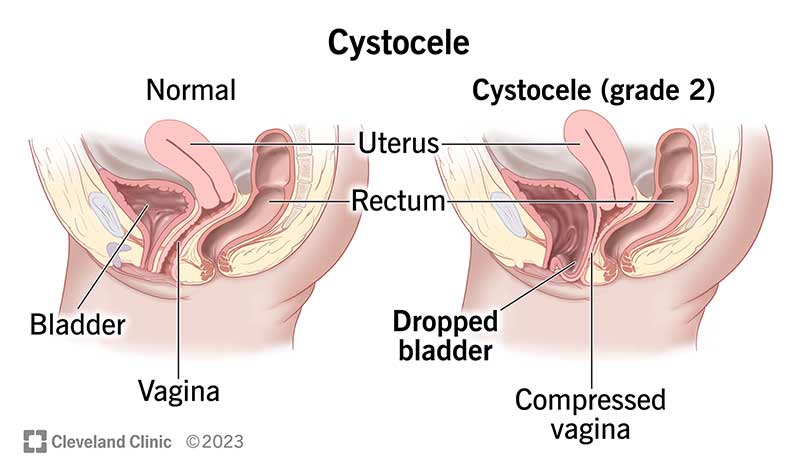
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15468-cystocele)
A cystocele is a condition in which the supportive ligaments and muscles around your bladder and vaginal wall that hold up your bladder stretch or weaken. This allows your bladder to sag into your vagina. It’s a type of pelvic organ prolapse.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Other names for a cystocele (SIS-tuh-seel) include:
There are three grades of cystocele:
It depends on the severity of your cystocele.
A mild cystocele may only cause discomfort or cause you to leak pee accidentally (urinary incontinence). A severe cystocele prevents you from being able to pee. This can cause an infection or kidney damage.
Cystoceles are common. Medical experts estimate that about 50% of women have some grade of cystocele.
Cystocele symptoms may include:
Advertisement
Stretched or weakened pelvic ligaments cause cystoceles. Many different factors can damage the ligaments. These include:
A cystocele can affect anyone with a vagina of any age. However, you’re more likely to have a cystocele as you age and your pelvic floor muscles weaken. The following can also increase your risk of developing a cystocele:
A cystocele can push on your urethra and prevent your bladder from completely emptying when you pee (urinary retention). It can also twist your ureters. Your ureters are two tubes that move pee from your kidneys to your bladder. A buildup of pee in your kidneys can cause kidney damage.
A healthcare provider who specializes in the female reproductive and urinary systems (urologist or gynecologist) can diagnose a cystocele. They’ll review your medical history, ask questions about your symptoms and conduct a physical examination.
The provider may also perform the following tests:
Only a healthcare provider can diagnose a cystocele. However, many may feel the bulge coming out of their vagina, and they can push it back in with their hands. If you have cystocele symptoms, see a healthcare provider immediately.
It depends on how severe your cystocele is.
If you have a mild cystocele that doesn’t bother you, you may not need any treatment other than to avoid heavy lifting or straining that could worsen the cystocele.
Other mild cystocele treatment options include:
Some moderate or severe cystoceles may require surgery if the above options don’t work.
A moderate or severe cystocele may require an anterior colporrhaphy. An anterior colporrhaphy is a type of reconstructive surgery in which a surgeon moves your bladder back into its normal position and tightens the muscles in the front wall that hold your bladder in place.
Advertisement
Cystocele surgery is usually an outpatient procedure, meaning you can go home the same day you have the surgery. Most people have a complete recovery in a few months.
If you never plan on having sexual intercourse again, there are surgical options that sew the vagina shut and shorten it so there are no longer any bulges.
If more than your bladder is falling down — such as your uterus, the top of your vagina (providers call this the apex after a hysterectomy) or the rectum — then your provider may discuss other types of surgeries with you.
For a severe cystocele that requires surgery, you should feel better soon after the surgery. But complete recovery may take a few weeks.
Cystoceles aren’t life-threatening, but they can negatively affect your quality of life. A cystocele can get worse without treatment. In the worst cases, you may not be able to pee, which can cause an infection or damage your kidneys.
It depends. You can control certain cystocele risk factors, including:
Advertisement
However, you can’t modify other risk factors, like your family history or age.
If you have a cystocele, you should avoid heavy lifting or any activities that put pressure on your pelvic floor muscles.
It’s also a good idea to prevent or treat chronic coughing. Avoid or quit smoking, and get treatment for conditions that cause a chronic cough, such as bronchitis. A long-lasting cough can put a lot of pressure on your chest and abdomen, which causes your pelvic floor muscles to strain.
Reach out to a healthcare provider if you have any symptoms of a cystocele, especially if they affect your quality of life.
Go to the emergency room if you have signs of a cystocele and can’t pee.
A prolapsed bladder and a cystocele are the same condition. Prolapsed bladder is another name for cystocele.
Cystoceles usually aren’t dangerous, but they can make you feel embarrassed or self-conscious. Don’t hesitate to contact a healthcare provider if you have cystocele symptoms that affect your quality of life. They’ll review your medical history and symptoms and suggest the best treatment options to repair your cystocele and improve your well-being.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
It can be stressful (and painful) to have bladder disorders, like urinary incontinence or cystitis. But the urology providers at Cleveland Clinic are here for you.
