A bowel obstruction is a partial or complete blockage of your small intestine or large intestine (bowels). The most common causes include scar tissue forming after abdominal surgery, hernias and colon cancer. A bowel obstruction is a medical emergency that requires immediate care.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
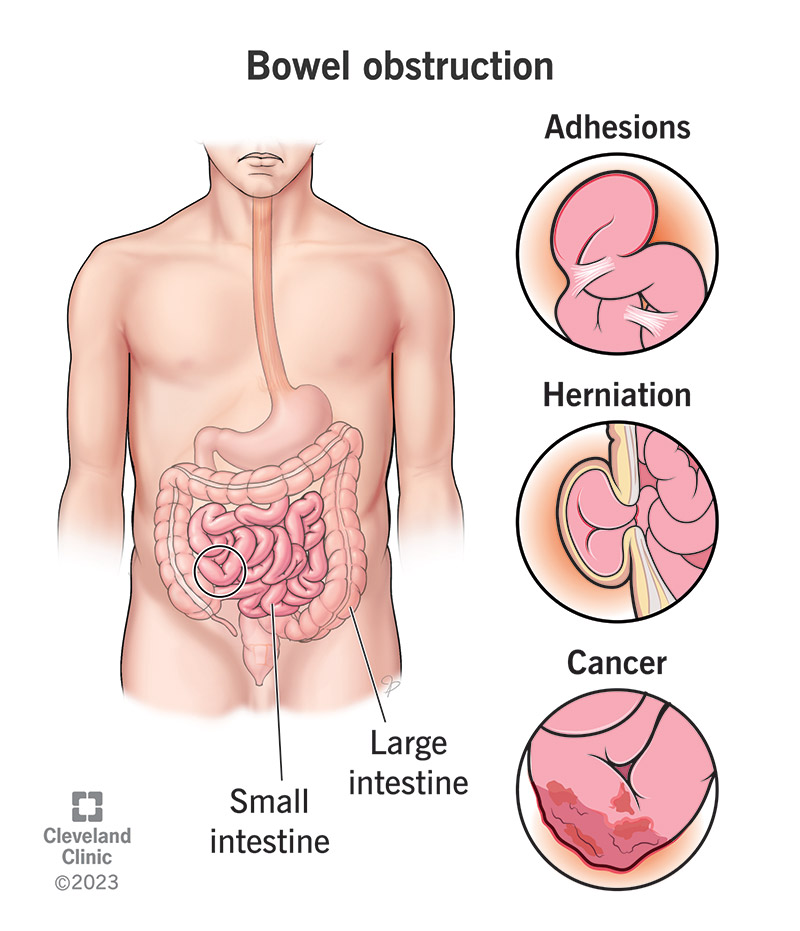
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/bowel-obstruction.jpg)
A bowel obstruction is a partial or complete blockage of either of your bowels — your small intestine or your large intestine. Your intestines move food and (eventually) food waste from your stomach to your rectum, which you pass as stool when you poop. An obstruction blocks your intestinal passageway, slowing movement or grinding digestive processes to a halt.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Waste, gas and digestive juices can get stuck behind the blockage, damaging the tissue. The blockage can prevent your bowel from working as it should, leading to dangerous complications.
With a bowel obstruction, time is of the essence. If you’re noticing symptoms of an obstruction, call a healthcare provider or get to an emergency department (ED) right away.
Healthcare providers classify bowel obstructions based on which intestine they affect:
Bowel obstructions can also be:
Advertisement
Small bowel (intestine) obstructions are a common reason people visit the ED.
Large bowel obstructions are uncommon in the general population, but they’re frequent among people with colon cancer. About 40% of people with colon cancer get diagnosed because bowel obstruction symptoms (from a tumor) prompted them to seek emergency care.
You may have sharp stomach pains that come in waves. Eventually, the pain may become constant. You may also have one or more of these symptoms:
Infants and children experience the same symptoms as adults. Infants can’t tell you where it hurts, but they may pull their legs up toward their bellies and cry. Other symptoms of bowel obstructions in children include:
A bowel obstruction can feel different depending on which intestine is affected and what’s happening in your gut.
An obstruction typically feels like severe cramping pain in your abdomen. The pain from a small bowel obstruction is more likely to come in short intermittent waves, occurring every few minutes or so. The pain is more likely to feel concentrated in one place.
The cramping from a large bowel obstruction tends to be more continuous. The pain is more likely to feel spread out.
Regardless of the specifics, if you’re having severe cramping alongside symptoms like bloating and vomiting, seek immediate care.
It’s possible. It depends on where the blockage is and how serious it is. For example, while pooping may be more difficult, you may still have stool with a partial bowel obstruction. Pooping and even passing gas will likely be impossible with a complete bowel obstruction.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_r61shnz2/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn what causes bowel obstructions.
The most common causes of bowel obstructions include:
Advertisement
Other causes of bowel obstructions include:
Advertisement
The complications of a bowel obstruction are life-threatening without emergency care.
As a bowel obstruction is a medical emergency, diagnosis usually happens quickly. It may happen alongside treatment, so no time is lost. Diagnosis may involve:
Advertisement
Imaging procedures allow your provider to view the obstruction and check for complications. These include:
These imaging procedures use radiation. You may need alternatives to these procedures if radiation exposure (even at safe levels) poses any potential risk. Children and women who are pregnant may need ultrasounds or MRIs, which don’t use radiation.
Most people with bowel obstruction need prompt treatment in the hospital. Complete obstructions usually require immediate surgery. Partial bowel obstructions may require treatments to stabilize your condition, followed by nonsurgical solutions, like bowel rest. It all depends on how severe the obstruction is.
Treatment may include:
Most people with bowel obstructions improve after treatment. Being able to pass gas again, feeling less bloated and being able to have bowel movements again are all signs your bowel obstruction is clearing.
On the other hand, if an obstruction causes a rupture, the condition can be life-threatening. It’s essential to seek care as soon as you notice symptoms to get treated before a complication happens.
Call your healthcare provider if you experience:
Questions to ask include:
If you’re noticing symptoms of a bowel obstruction, act fast to seek care. In general, many people wait out pain, worrying that seeing a provider is an overreaction. But when it comes to a bowel obstruction, “toughing it out” is never a good option. Take abdominal pain seriously, especially if you’ve had previous abdominal surgery or if you have a condition that increases your risk, like IBD. An obstruction is a treatable condition that you can recover from with prompt medical attention. Don’t delay.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Some conditions like rectal and colon cancer, Crohn’s disease and ulcerative colitis may require colorectal surgery. Cleveland Clinic has the expert care you need.
