Hirschsprung’s disease is a condition your baby is born with (congenital) that makes it hard for them to poop. If left untreated, it can lead to constipation and bowel obstruction, which can be dangerous. Sometimes, Hirschsprung’s disease affects older children or adults, but it’s very rare.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
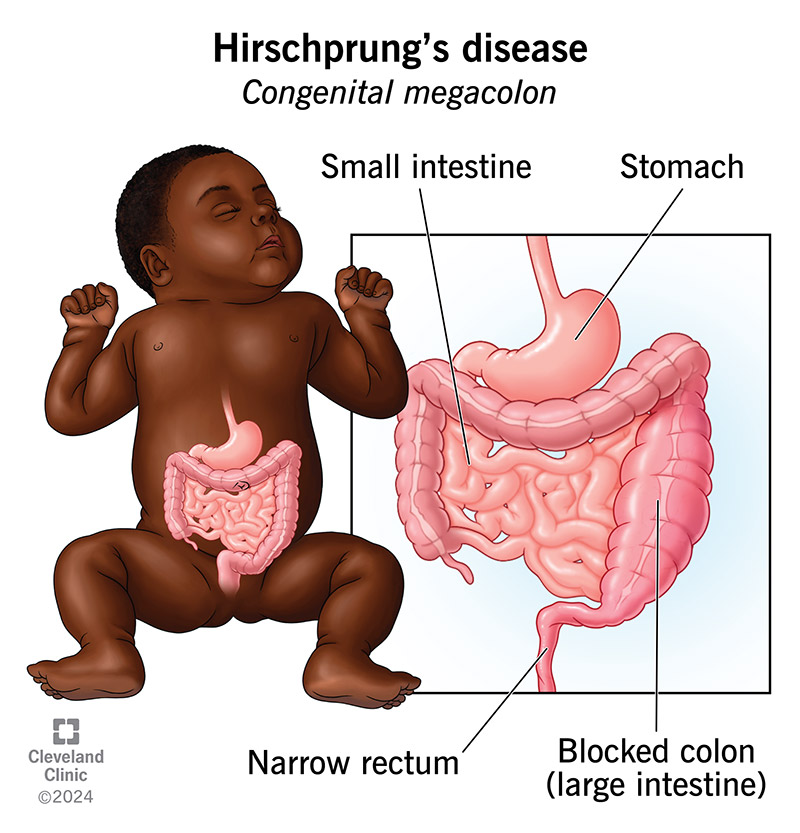
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/9844-hirschprungs-disease.jpg)
Hirschsprung’s disease is a condition your child is born with (congenital) that slows or stops the movement of waste (poop) through their colon. Your child’s healthcare provider may also call it congenital megacolon. In Hirschsprung’s disease, nerve cells don’t develop as they should near the end of your baby’s large intestine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When digestion happens as expected, nerve cells send signals telling muscles in your colon to tense and relax. These specific nerve cells are called neural crest cells. This tensing and relaxing moves waste (poop) along, from the beginning to the end of your intestines. Eventually, the waste fills your rectum, which activates nerves in the lining of your anus (butthole) that make it feel like you have to poop.
If your baby has Hirschsprung’s disease, poop moves through their intestines until it reaches the section that’s missing nerve cells. Once the poop reaches that point, it moves slowly or stops (constipation).
Without treatment, Hirschsprung’s disease can cause serious complications.
Hirschsprung’s disease occurs in about 1 out of 5,000 births. It is three to four times more common in males.
Some babies with Hirschsprung’s disease have blocked intestines at birth. There’s a chance your baby has Hirschsprung’s disease if they don’t poop within 48 hours after birth.
Other symptoms of Hirschsprung’s disease in babies may include:
During fetal development, neural crest cells typically grow from the top of the small intestine through the large intestine to the anus. In children with Hirschsprung disease, these nerve cells stop growing in the large intestine before reaching the anus. Healthcare providers aren’t sure why this happens.
Advertisement
Less than 20% of the time, Hirschsprung’s disease runs in families. A change in a gene (genetic mutation) may be the cause.
Aside from having a biological parent or sibling with the condition, risk factors for Hirschsprung’s disease include having:
Up to 40% of children with Hirschsprung’s disease develop enterocolitis. This condition is the swelling of your child’s small and large intestines. Some children have mild inflammation. Others have severe symptoms that can be life-threatening. If your child has severe enterocolitis from Hirschsprung’s disease, they may have fever and explosive diarrhea.
Severe or untreated Hirschsprung’s disease can lead to these potentially life-threatening problems:
Other complications include:
Your baby’s healthcare provider will check their belly to see if it’s swollen and painful. Then they’ll check your baby’s rectum for backed-up poop.
Your child’s provider may also perform one or more of these tests:
There’s no cure for Hirschsprung’s disease, but surgical treatment often results in a positive outcome. There are two types of surgeries to treat Hirschsprung’s disease: a pull-through procedure and an ostomy.
Advertisement
A surgeon removes the section of your baby’s large intestine that’s missing nerve cells. Then they connect the healthy part of your baby’s large intestine to their anus. The surgeon may use laparoscopic or traditional surgery to perform the pull-through procedure.
The pull-through procedure is the most common surgery for Hirschsprung’s disease and has the best outcome for recovery.
Your baby may need a colostomy (large intestine) or ileostomy (small intestine) before, or at the same time as, a pull-through procedure.
During ostomy surgery, surgeons connect the large or small intestine to the skin outside your baby’s belly. Ostomy surgery allows poop to leave your baby’s body through an opening (stoma) outside of your baby’s anus, usually around their belly. The poop goes into an ostomy bag attached to your baby’s body.
Some nonsurgical treatments work well in addition to surgery. They include:
Advertisement
Children with Hirschsprung’s disease often feel much better soon after pull-through surgery. But some children may still have problems after they heal, including:
Your baby’s surgeon and sometimes a gastroenterologist will help with the management of these problems.
If everything goes well, your baby will feel much better a few days after surgery.
There’s no cure for Hirschsprung’s disease, but surgical treatment often results in a positive outcome. There are two types of surgeries to treat Hirschsprung’s disease: a pull-through procedure and an ostomy.
After surgery, some babies with Hirschsprung’s disease may still have constipation, pooping accidents and colon infections. But with long-term follow-up care, most children can manage pooping without becoming severely constipated or developing fecal incontinence.
No one can prevent Hirschsprung’s disease. If you have the disease or a family history of it, you may want to meet with genetic counselors before starting a family.
Treatments that can help your child manage Hirschsprung’s disease after surgery include:
Advertisement
Talk with your child’s healthcare providers. They’ll work with you to figure out the best foods and therapies to help your child overcome any challenges.
Children can get enterocolitis in their intestines after surgery, especially in the first year. Call the doctor right away if your child shows any of these symptoms:
Just because your baby is born with Hirschsprung’s disease doesn’t mean they won’t live a happy and healthy life. Surgery is used to treat the disease, but the time leading up to the surgery can be stressful.
You’ll need to watch your baby carefully for signs of intestinal blockage. This time can be especially challenging since you’ve just had a baby. It’s not unusual to be sad or scared. Lean on your family and friends for support when you need it. Let them do the laundry and help with chores at home or meals so you can spend time with your baby or take a nap.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have issues with your digestive system, you need a team of experts you can trust. Our gastroenterology specialists at Cleveland Clinic can help.
