Interstitial cystitis/bladder pain syndrome is a condition that causes long-term pain or discomfort in your bladder and abdominal area, along with urinary frequency and urgency. Healthcare providers don’t know what exactly causes it. But potential causes may include autoimmune diseases, allergies and issues with your bladder lining.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
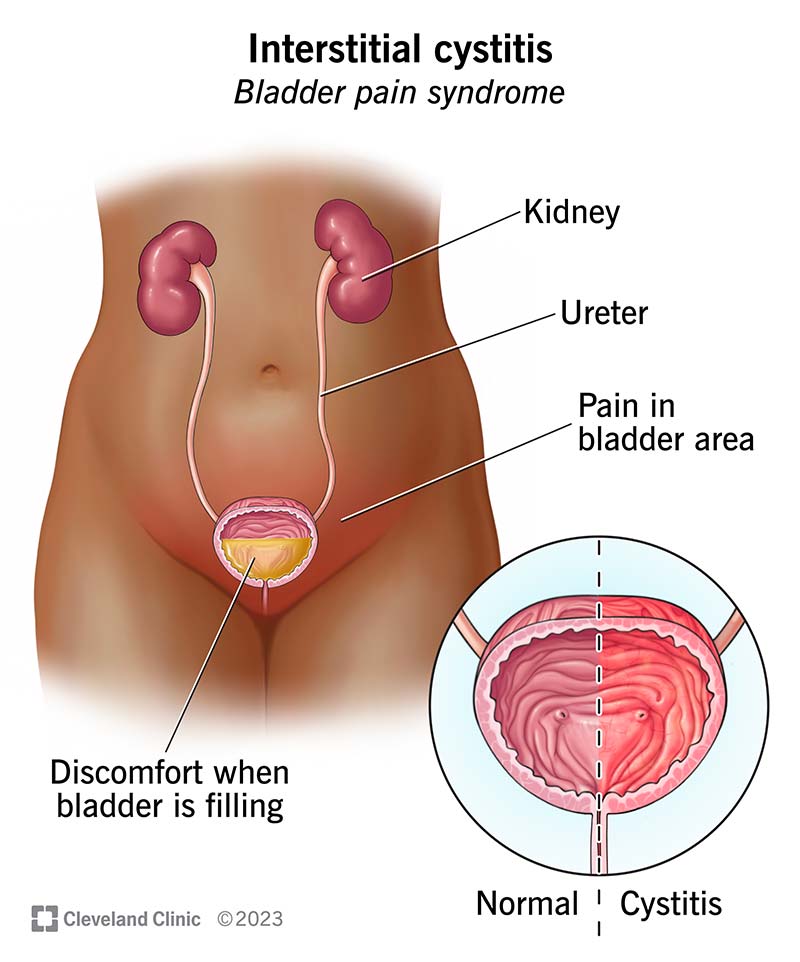
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/interstitial-cystitis)
Interstitial cystitis — now known as bladder pain syndrome (IC/BPS) — is long-term (chronic) discomfort, pain or pressure in your bladder area (suprapubic region). “Interstitial” means it affects the spaces between your tissues or organs. “Cystitis” means inflammation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If you have IC/BPS, you need to urinate (pee) more often than usual (frequency) and feel like you have to pee right away (urgency).
Other names for interstitial cystitis include:
There are two types of interstitial cystitis/bladder pain syndrome:
Stage 4 interstitial cystitis/bladder pain syndrome is when you have continuing IC/BPS symptoms for over two years. Your bladder tissue becomes very hard and can’t hold as much pee. Stage 4 IC/BPS most commonly affects people who have Hunner’s ulcers.
Interstitial cystitis/bladder pain syndrome is common. In the U.S., it affects approximately:
Interstitial cystitis/bladder pain syndrome symptoms vary. They may be mild or severe. They may also be constant or only appear occasionally. Symptoms include:
Advertisement
If you’re a woman, your symptoms often get worse when you’re menstruating.
Interstitial cystitis/bladder pain syndrome may feel different from person to person. You may only feel mild discomfort. Or you may feel a lot of pain and sudden, frequent urges to pee.
Healthcare providers and medical researchers don’t completely understand what causes interstitial cystitis/bladder pain syndrome. They suspect that it may relate to certain medical conditions, including:
Anyone can get interstitial cystitis/bladder pain syndrome. But you may be at a greater risk of getting IC/BPS if you:
There aren’t any specific tests to diagnose interstitial cystitis/bladder pain syndrome. However, a healthcare provider will order tests to rule out other infections or conditions. These tests may include:
Advertisement
You can’t fix or cure interstitial cystitis/bladder pain syndrome. But there are many ways to treat it. The goal of IC/BPS treatment is to relieve your symptoms. A healthcare provider will work with you to decide the most appropriate treatment. They may even combine treatments.
Providers can’t predict how you’ll respond to each treatment. You’ll go through a trial-and-error process with various treatments to see how your body responds. Your symptoms may go away, or they may become more severe. Even if your symptoms disappear, they may return later.
IC/BPS treatments may include:
Some people who have IC/BPS report that certain foods and drinks worsen their symptoms (triggers). Keep a diary or journal of what and how much you eat and drink each day. Noting what you eat and drink before your symptoms start and/or a flare-up can help you learn what foods and drinks to avoid.
If you notice that acidic foods and drinks — for example, citrus fruits, peppers, carbonated beverages and tomatoes — cause flare-ups, a provider may recommend taking an antacid with meals. Antacids reduce the amount of acid that gets into your pee.
Common foods and drinks that may cause IC/BPS symptoms include:
Advertisement
A provider may refer you to a dietitian to help you create the best eating patterns to reduce IC/BPS symptoms.
Exercise and physical activity may help relieve IC/BPS symptoms, including:
Stress may trigger IC/BPS flare-ups. Learning to recognize and manage stress may help alleviate your symptoms. Talking to a mental health professional (psychotherapy) can help you reduce stress.
Your pelvic floor muscles hold your bladder in place and help control when you pee. Strengthening (Kegel exercises), stretching and especially relaxing your pelvic floor muscles can help relieve interstitial cystitis/bladder pain syndrome symptoms. A provider can help ensure you’re performing these exercises correctly. Many people work with a pelvic floor physical therapist to make sure they’re properly relaxing their pelvic floor muscles.
If you have bladder pain, it’s easy to get into the habit of using the bathroom as soon as you feel pain or urgency, even if your bladder isn’t full. Your body conditions itself to go to the bathroom more often. Bladder retraining helps you overcome this habit by training you to hold your pee for longer periods.
To practice bladder retraining, keep a diary or journal of how often you pee and how often you have the urge to pee. Use your diary or journal to help you gradually increase the time between bathroom breaks.
Advertisement
The following oral medications may help treat IC/BPS symptoms:
A provider will insert a thin, plastic tube (catheter) in your urethra and guide it up to your bladder. They’ll then fill your bladder with a mixture of medications that may include dimethyl sulfoxide (DMSO), a steroid and a numbing medication. DMSO is a liquid medicine that helps alleviate symptoms.
A provider fills your bladder with sterile water to stretch out your bladder. This increases the amount of pee your bladder can hold. Hydrodistension may also calm or break the overactive nerve endings that tell your brain your bladder is in pain. You’ll receive anesthesia during hydrodistension so you’re asleep and won’t feel any pain during the procedure.
Nerve stimulation (neuromodulation therapy) regulates your bladder by reducing urgency and frequency. It uses electrical stimulation to stimulate your nerves and produce a response. It sometimes helps alleviate pain in your bladder and abdominal area.
A provider injects botulinum toxin (Botox®) into your bladder muscle through a cystoscope. Small amounts of Botox paralyze the muscle and alleviate pain. You may need Botox injections every four to nine months.
A provider may recommend surgery if you have severe IC/BPS symptoms and don’t respond to other treatments. They may remove part or all of your bladder (cystectomy).
In addition to treating your bladder and pelvic floor, a provider will consider other conditions that may cause part of your pain, including:
It depends. Most people who have interstitial cystitis/bladder pain syndrome need treatment for their entire lives. If they don’t get treatment, their symptoms may return. They may even have flare-ups while they’re actively treating IC/BPS.
Some people respond well to treatment. Their symptoms slowly improve and even go away.
Talk to a healthcare provider. They can tell you what treatments may offer the fastest relief for your IC/BPS symptoms.
It may take several weeks or months before your symptoms start to improve after IC/BPS treatment.
For many people, interstitial cystitis/bladder pain syndrome is a long-term condition. Your symptoms may be mild or severe. They may appear only occasionally, or they may be persistent.
Talk to a healthcare provider to help determine your outlook and the best treatment options.
Interstitial cystitis/bladder pain syndrome isn’t a life-threatening condition. It doesn’t cause bladder cancer and won’t affect your life expectancy.
Healthcare providers and medical researchers don’t know how to reduce your risk of developing interstitial cystitis/bladder pain syndrome or prevent symptoms from recurring. You may be able to prevent flare-ups by:
The following may help reduce the length and severity of your interstitial cystitis/bladder pain syndrome flare-ups:
Schedule an appointment with a healthcare provider if you have symptoms of interstitial cystitis/bladder pain syndrome. A provider will order tests to rule out infections or other conditions that may cause IC/BPS symptoms. They may also recommend or prescribe medications.
Go to the nearest emergency room if your symptoms are severe or don’t go away after treatment.
It may be helpful to ask your provider:
People sometimes mistake interstitial cystitis/bladder pain syndrome for a urinary tract infection (UTI). But IC/PBS and UTIs aren’t the same. Microorganisms (usually bacteria, especially E. coli) cause UTIs. Healthcare providers don’t yet understand what causes IC/BPS. But medical conditions that may relate to IC/BPS include autoimmune diseases, allergies and problems with your blood vessels.
Interstitial cystitis/bladder pain syndrome is a common, chronic condition that causes inflammation and discomfort in your bladder area. It also affects your peeing habits — you may pee more often during the day, and when you have to go, it’s urgent. Pain, discomfort and problems peeing can make you feel self-conscious. But don’t be embarrassed to talk to a healthcare provider if you have signs of IC/BPS. They can order tests to rule out other conditions. They can also work with you to develop the most effective treatment plan that will reduce the length and severity of your flare-ups and increase your quality of life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
It can be stressful (and painful) to have bladder disorders, like urinary incontinence or cystitis. But the urology providers at Cleveland Clinic are here for you.
