Acute coronary syndrome (ACS) refers to a group of conditions that involve sudden, reduced blood flow to your heart. This happens due to a partial or complete blockage in one of your coronary arteries. Common symptoms include chest pain or pressure (angina), shortness of breath and dizziness. ACS is a medical emergency that needs prompt treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
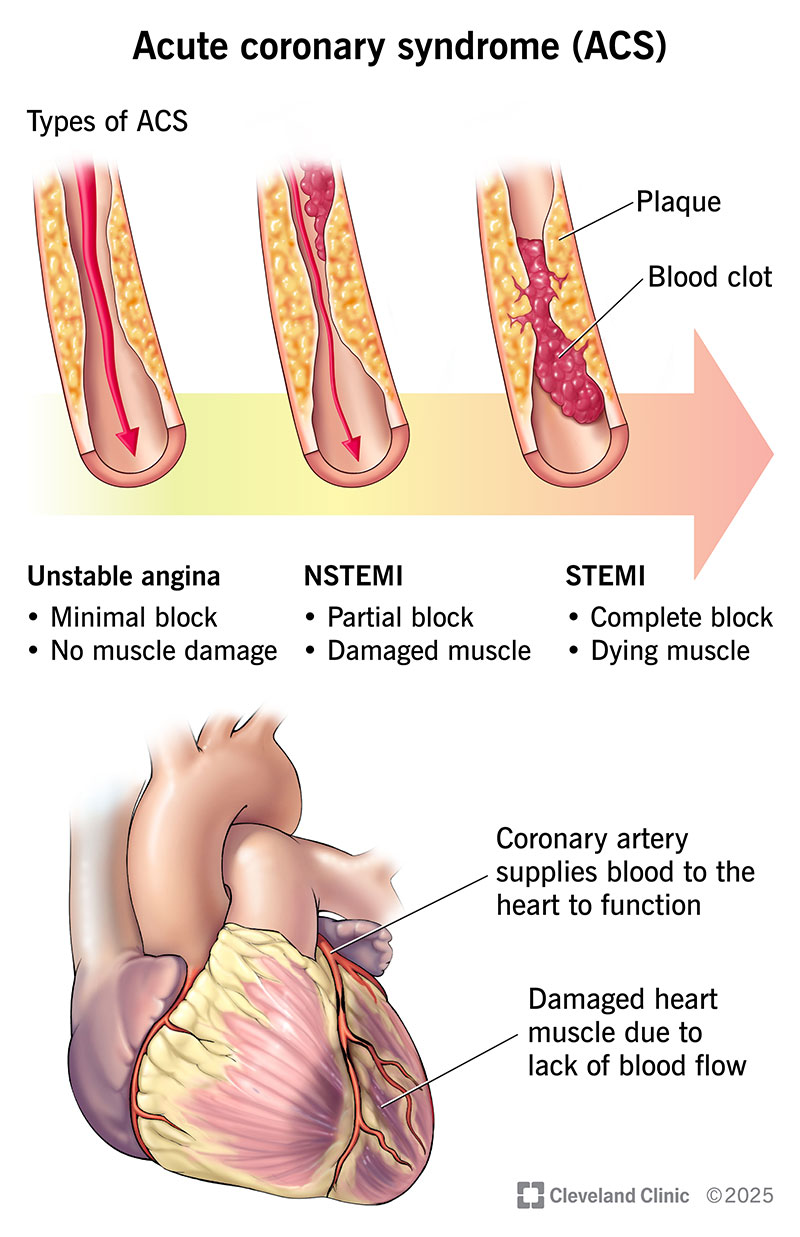
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22910-acute-coronary-syndrome)
Acute coronary syndrome (ACS) is an umbrella term that includes unstable angina, STEMI heart attacks and NSTEMI heart attacks. With all these conditions, a blockage in a coronary artery reduces blood flow to your heart muscle. This means your heart isn’t receiving the blood it needs to work as it should, which could result in irreversible damage to your heart or even sudden cardiac death. You need treatment right away to open the artery and prevent or limit heart damage.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Acute coronary syndromes are life-threatening. Call 911 or your local emergency number right away if you have heart attack symptoms or your angina suddenly feels different than usual. Tell the operator what you’re feeling. Ask if you should take an aspirin.
There are three acute coronary syndromes:
It’s possible for unstable angina to quickly turn into a heart attack. And for an NSTEMI to turn into a STEMI.
ACS symptoms typically occur without warning, even while you rest. You might have:
Advertisement
It’s not always easy to tell if chest pain comes from your heart or something else, like acid reflux. That’s why you should always seek medical care for sudden chest pain. Don’t try to guess the cause or wait it out. If it’s an acute coronary syndrome, every minute can make the difference between surviving and not.
A blood clot in your coronary artery causes ACS. This is generally due to cholesterol plaque rupturing inside your artery, but it can happen due to blood clots coming from other sources. The clot partly or completely blocks the space where blood can flow. This means your heart can’t get enough blood. Severe blockages can damage your heart muscle or even be fatal.
You may develop an acute coronary syndrome if you’re living with coronary artery disease. This means you have cholesterol plaque buildup in your arteries. The plaque gradually narrows your arteries over many years. This may cause stable angina, or chest discomfort that comes and goes in predictable patterns, usually when you exercise or are physically active. Your provider may give you medicine to treat these episodes.
But things can quickly change if the surface of that plaque wears away (plaque erosion) or breaks open (plaque rupture). When the plaque ruptures or erodes, blood clots form at the spot and reduce blood flow, leading to unstable angina or a heart attack.
You’re more likely to develop ACS if you:
Healthcare providers diagnose acute coronary syndromes using a physical exam, blood tests and an EKG, which records your heart’s electrical activity. The results show whether your condition is a heart attack or unstable angina. Providers also review your medical history, including any medications you’re taking.
Further tests can help rule out other conditions and guide treatment. Possible tests you may need include:
Advertisement
If results show that blood flow to your heart is blocked, you’ll receive immediate treatment.
Providers may ask you questions if you’re able to speak. They’ll want to know about your symptoms. The more details you can provide, the better. Consider:
ACS treatment needs to happen fast. The longer a blockage lasts, the greater your risk of heart damage or death. Treatments involve medicines and procedures that open your coronary arteries to improve blood flow to your heart. You may also need medicines to help your heart work better, manage symptoms and lower your risk of complications.
Treatments that open up blocked arteries include:
Advertisement
Medicines you may need include:
How long it takes to recover from an acute coronary syndrome depends on the specific condition you have. In general, you may need several weeks or months to feel better.
Follow your healthcare provider’s advice as you recover. Don’t push yourself to get “back to normal” too fast. Your provider will tell you when it’s safe to return to usual tasks, like driving, working or lifting heavy objects. They might also recommend that you engage in a cardiac rehabilitation program for monitored exercise after you’ve had an ACS.
You’ll need to see your provider for regular follow-up appointments and testing. They’ll give you a schedule of when to come in. These visits are crucial as you recover. Your provider will:
Advertisement
Be sure to tell your provider if:
It’s common to feel depressed or anxious after having a heart attack or coming close to one. Your provider may recommend counseling or support groups. These can help you learn practical tips for managing any emotions you’re feeling.
Call 911 or your local emergency services number if you think you’re having unstable angina or a heart attack. Don’t drive yourself to the hospital or let anyone else drive you. First responders are prepared to start treating you as soon as they arrive and while you’re in the ambulance. This saves valuable time and can even be lifesaving.
Your outlook depends on whether you have unstable angina or a heart attack — and if it’s a heart attack, how severe it is. Unstable angina usually doesn’t damage your heart muscle. But a heart attack can. A STEMI typically causes more damage than an NSTEMI.
Your healthcare provider is the best person to tell you what you can expect. In general, treatments have come a long way over the years. Many people live just as long as others their age who don’t have an acute coronary syndrome. You can improve your chances of survival by going to your follow-up visits and sticking to your treatment plan.
It’s not always possible to prevent ACS. You can’t change many things, like age or family history. But there are some steps you can take to lower your risk:
Acute coronary syndromes are serious — but with quick treatment, there’s a good chance you’ll be OK. The key is to call for help right away. It’s also vital to keep seeing your provider for regular follow-ups. If you’re living with stable angina, make sure you talk to your provider about which symptoms should make you seek care.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you need treatment for coronary artery disease, you want expert care. At Cleveland Clinic, we’ll create a treatment plan that’s personalized to you.
