Left Atrial Appendage Closure Preventing Strokes in Patients with Atrial Fibrillation
Subscribe: Apple Podcasts | Buzzsprout | Spotify
Left Atrial Appendage Closure Preventing Strokes in Patients with Atrial Fibrillation
Podcast Transcript
Announcer: Welcome to Love Your Heart, brought to you by Cleveland Clinic's, Sydell and Arnold Miller Family Heart And Vascular Institute. These podcasts will help you learn more about your heart, thorasic and vascular systems, ways to stay healthy and information about diseases and treatment options. Enjoy.
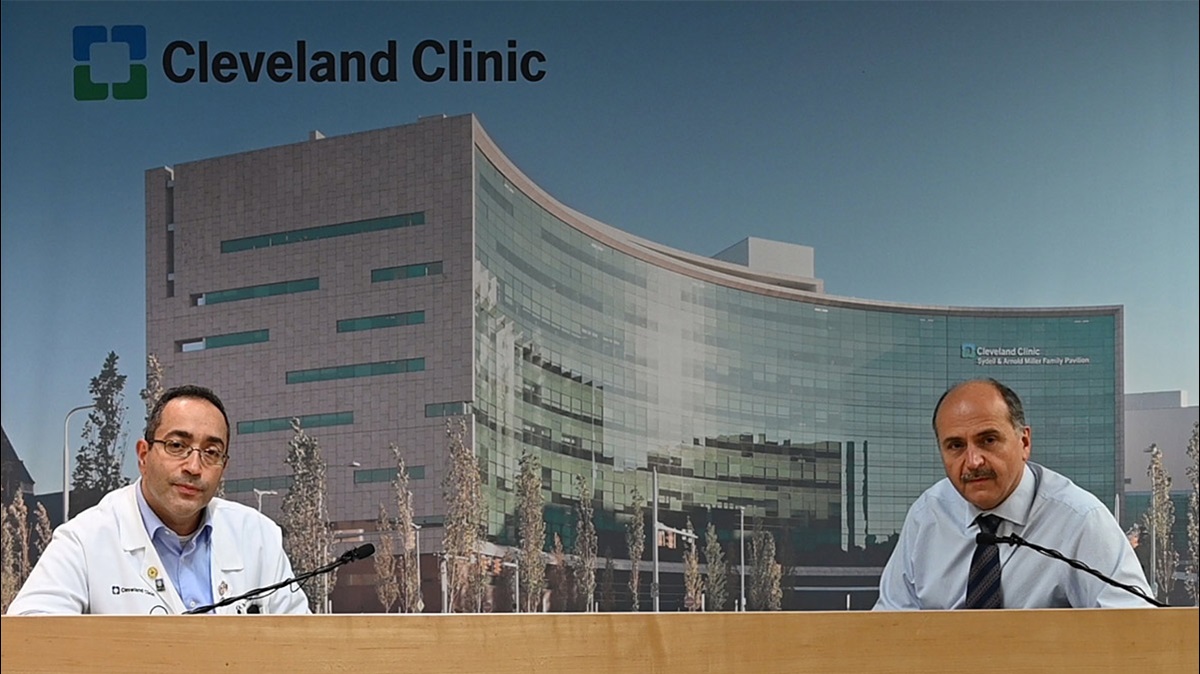
Dr. Oussama Wazni: Hello, I'm Oussama Wazni, I'm the section head of electrophysiologists at the Cleveland Clinic and here with me today is Dr. Walid Saliba. He's the director of the EP lab and also co-director of the Afib Stroke Prevention Center that we founded here at the Cleveland Clinic a few years ago. We're here to talk to you about left atrial appendage closure device. So without further ado, we'll start. Dr. Saliba, can you just tell us a little bit about the background of why you think this technology, or this aspect of patient care is as important as we found it to be?
Dr. Walid Saliba: Sure. As you know, atrial fibrillation increases the risk of stroke significantly and around five times increased risk of stroke in patients who have atrial fibrillation. And we also know that most strokes that occur in patients with atrial fibrillation, the clot is attributed to a clot in the left atrial appendage. Therefore it is very reasonable to think that if there is a some kind of a technology that allows us to block the left atrial appendage, that we would presumably decrease the risk of stroke. The studies that were actually done previously in the surgical literature, even though they were not randomized study, there were some points that this might be true. Finally with the advent of the left atrial appendage occlusion device, the WATCHMAN device, there were several studies that were done that actually proved that theory to be somehow right.
So we have at our disposal so far, several studies that two patients with atrial fibrillation at high risk of stroke as judged by a certain characteristics that they have based on the CHADS-VASc score, or the CHAD score. These patients were randomized into two, one fashion to either receive the WATCHMAN device, left atrial appendage occlusion, versus warfarin. So therefore these patients had to be able to take oral anticoagulation, which is very important for our discussion later. All those studies showed that the WATCHMAN device was not inferior to warfarin in terms of its efficacy in decreasing the combined endpoint of stroke or systemic embolization.
Also if you take the totality of the trials that was done, you can see that there was a significant, actually, reduction not only in the old cause of stroke but also in cardiovascular mortality, which was mainly driven by a reduction of risk of bleeding and bleeding events, which is essentially logical to think about because if patients have a WATCHMAN device to decrease their risk of ischemic stroke and therefore will not need to take longterm anticoagulation, which is the taboo of the old anticoagulants, then they will have a reduction in risk of hemorrhage.
Dr. Oussama Wazni: So who are the indicated patients today? Sorry, FDA indication today?
Dr. Walid Saliba: So the FDA indication, which I think is a reasonable wording because they had to base their indication on the kinds of patients that were enrolled in the studies, patients who had atrial fibrillation who are at an increased risk of stroke based on their CHADS-VASc score, which is a two or more, who are able or judged by the physicians to be able to take oral anticoagulation. This is also subjects for some controversy here, but they have an appropriate rationale to seek a non-pharmacological alternative to that reduction in risk of stroke, taking into account the risk and benefits of these alternatives.
Dr. Oussama Wazni: So can you tell us a little bit about how you developed the program at the Cleveland Clinic specifically for stroke prevention in atrial fibrillation patients?
Dr. Walid Saliba: So we realized early on during the development of such a center that most of the patients who will be seeking this kind of a therapy are the patients who do not, or cannot, take oral anticoagulation. So these are the patients who have had history of bleeding, yet they are at the high risk of stroke and they need to have some kind of prevention for stroke. These are the patients who are potentially bleeders who, because of certain characteristics being their job, their occupation, or certain medical conditions that they have, are at an increased risk of bleeding but they haven't bled yet.
With this in mind, we knew that those kind of patients that are of concern in these situations are the patients who had either bleeding in their head, bleeding in their gastrointestinal system, bleeding in genitourinary system and therefore we went ahead and partnered with our colleagues in the Neurovascular Institute and the Gastrointestinal Institute because we wanted to build more of a collaborate, multidisciplinary approach to this kind of a problem. So that when a patient comes to us, instead of flip-flopping from one clinic to another, we'll have a streamlined, one-stop approach so that when they come to us, they see us, we determine the risk of bleeding, we determine the risk of stroke. Based on the risk of bleeding, we send them to that clinic, so that our colleague will help us in determining what is the appropriateness and the risk of initiating anticoagulation on the short term for these patients?Because in order for us to put their device in, these patients need to be on anticoagulation around 45 days after the procedure.
Dr. Oussama Wazni: So, those are the patients, basically who were contraindicated, or were not included in the studies. Those are patients who already had a bleeding episode, or are very high risk for having bleeding. So can you tell us about our experience, or your experience in those kinds of patients?
Dr. Walid Saliba: That is a very important question because if you look at that group of patients, you can see that these are not the patients that typically were enrolled in the studies, but these are the patients who we think would have the most benefit, would derive the most benefit from the left atrial appendage occlusion device. So most of the patients that we have considered in our practice here are patients who actually have had either an intracranial bleed, or a subdural hematoma, or patients who had GI bleeding.
So these are patients at high risk of bleeding, definitely. Then we asked our colleague, is it okay to anti coagulate these patients for six to seven weeks, only to be able to put that device in? There was a lot of talk and then there was a lot of give and take and it's an experience for them as much as an experience for us. To our surprise, and very pleasantly so, those patients we were able to give them intermediate term anticoagulation. We have approximately now 50 patients and we published our data on 30 or 40 of these patients. We were able to get them on anticoagulation, put the device in, get them off anticoagulation with successful device implant in all of them. Most importantly, we have not had any problems with bleeding in any of these patients, except for one patient who actually had a traumatic bleeding after he stopped anticoagulation. So that was an eye-opener for us that this is something actually that is feasible, that this is something that we will have to reproduce in larger clinical trials.
Dr. Oussama Wazni: So this is very reassuring and I just want to emphasize the point that these are the patients who probably get the most benefit from left atrial appendage closure because we're able to close the appendage, decrease the risk of stroke, while at the same time not putting them at high risk for longterm anticoagulation and deep bleeding in the future.
Dr. Walid Saliba: Because the alternative is that if you're not going to give them anticoagulation and you're going to deprive them the luxury of having a device in, then their risk of stroke is quite significant.
Dr. Oussama Wazni: Yeah, and I think actually that our group has been the major leader in this kind of approach for these patients. How about the patients? So the problem with the studies, and that's why people are, I don't want to say resistant, but hesitant to implant the device as primary therapy and not in bleeders is because, the device was not superior to warfarin in terms of decreasing the risk of a cerebral ischemic stroke or embolism. But I know that you just shared with me that we have some data on very high risk patients with the high CHADS-VASc. So can you tell us about that Group of patients?
Dr. Walid Saliba: We have so far for the past few years we've implanted in excess of 300 such devices. So if we pull out the patients who have a high risk of stroke, these are patients who have a CHADS-VASc score of five and above and you look at ... and two third of these patients have had a history of stroke or TIA.
Dr. Oussama Wazni: Yes.
Dr. Walid Saliba: So we're talking secondary prevention now, of stroke. If you look at what happened to those patients after we've implanted that WATCHMAN device, first of all, we were able to implant the WATCHMAN device in all of them. Then when you follow them up, their risk of stroke after they had gone through the 45 days of anticoagulation and stopping is only 2.8%. if you compare that to a historical control with the CHADS-VASc of five to six their risk of stroke or systemic embolization is an excess of 12% and with warfarin alone, assuming it's 70% to 80% reduction in risk of stroke, that risk was down only to 4%. So those patients who've had a stroke before, high CHADS-VASc, very high risk, who have had also probably bleeding problems. Instead of leaving leaving them alone, we were able to get them down to a 2.8% risk of stroke with the WATCHMAN device.
Dr. Oussama Wazni: This is very reassuring meaning and showing that actually the therapy works in decreasing the risk of ischemic stroke or embolization because that was the concern we had from protect and prevail because in those studies it was just equivalent to warfarin, without being superior to warfarin in decreasing ischemic stroke. But based on the very high risk patients, our cohort, it looks like it does work even better in the higher risk patient.
Dr. Walid Saliba: Exactly, and if you look at some of the subgroup analysis in protect for looking at patients who've had prior history of stroke, so those secondary prevention patients it did, even though it was not a pre-specified endpoint, but it did decrease actually the risk of ischemic stroke in those patients, which is very important. Now one more thing that we have to add for those very high risk patients, who also have high risk of bleeding because this is the kind of patients that we have implanted. These patients in the community might be left alone.
Dr. Oussama Wazni: Yes.
Dr. Walid Saliba: When you are faced with the risk of bleeding with intermediate term anticoagulation, which is very low in our experience, versus the risk of stroke, if you are not taking anticoagulation, it becomes a no-brainer that this is the way that things needs to be actually moving.
Dr. Oussama Wazni: I know also that there was a new iteration of the WATCHMAN device that has been in clinical trials. Can you tell us a little bit about it and how is it different from the original WATCHMAN?
Dr. Walid Saliba: So the original WATCHMAN device has its own limitations, mostly size limitations. If the appendage is too small, the current available older WATCHMAN devices cannot actually be used for these appendages. Or if the anatomy of the left atrial appendage whereby the [intangible] is too large and the appendage is too short, the currently available WATCHMAN device, approved WATCHMAN device, cannot be used. Therefore, there's a new iteration of the WATCHMAN device where there are certain changes, such as now you can use that newer device for smaller appendages or for short appendages, or for larger appendages.
Also the technique to put it in place is probably more comfortable for physicians to use because it doesn't have those feet at the tip. It has a closed end that is there, and therefore you can form a little bit of a ball and push it. It gives you also more flexibility in terms of implant technique. With the older device, if you put it proximal and you're not happy with that, then you have to retract the device, throw it away, get a new device in its place. Whereas that new device allows you to partially retract it and then push it forward. So more flexibility in terms of the implant procedure for the implanting physicians.
Dr. Oussama Wazni: Excellent. And how about the Amulet device? I know it's in studies. Where is that going, you think?
Dr. Walid Saliba: Well, there are a lot of other devices that are going to be in clinical trials and now that the WATCHMAN is approved, it's easier to get those devices on the market. All they have to do is actually compare it to the available WATCHMAN du jour, and it is in clinical trial. We are a part of this clinical trial. It does have its advantages in terms of implantation, ease of implantation. We'll have to wait for the major clinical trial in the US, to see what is the outcome going to be, but we know from a clinical experience in Europe that the efficacy and the safety of that device might be comparable to the available WATCHMAN, but this is something that we will need to actually establish here, yes.
Dr. Oussama Wazni: How about the safety profile of our own experience with WATCHMAN at the clinic so far?
Dr. Walid Saliba: So we are very excited about our experience because we have had in excess of 300 implants. Most, importantly because there was a concern with the initial experience with the protect Afib, that there might be a high risk of adverse outcome at the time or very procedurally. We have not had any device embolization with the WATCHMAN.
Dr. Oussama Wazni: That's nice, yes.
Dr. Walid Saliba: We have not had any pairing device implantation strokes. We have had one case of delayed pericardial effusion without tamponade that we elected to a drain percutaneously and our experience, despite the fact that there's probably four of us who do these kind of implantations, have had very good experience and not having any problems.
Dr. Oussama Wazni: That's actually impressive because even comparing to the controlled studies, the risk of effusion was much higher than one in 300, that was probably more around 1% to 2% in the later iterations actually of the studies. So basically what we're saying, is that it is very effective in decreasing the risk of ischemic stroke and definitely decreasing the risk of bleeding and it has a very good safety profile. So what would it take for you in your mind, for us to start offering left atrial appendage closure as first line therapy, without having the patients having to have an intracranial hemorrhage before we offer them this device?
Dr. Walid Saliba: So that is a very important question. We have always to remember that the major clinical trials that were done with the WATCHMAN device were against warfarin. Warfarin has its potential problems in terms of time and therapeutic range in terms of a patient not discontinuing the medication. So with the new kids on the block, which are the newer anticoagulants, which have proven actually some superiority in certain respect to warfarin, the question is what is it going to take for us to suggest the device therapy versus newer anticoagulant therapy? So we will have to see how these two actually compare, because I think that the main alternative treatment option now that is available for stroke prevention is with the increasing use of the newer anticoagulant versus the WATCHMAN. Also, we have to keep in mind what kind of patient population was included in the study for the WATCHMAN.
These are patients who, their highest risk of stroke is really from the left atrial appendage. So these are patients who do not have aortic arch atherosclerosis, do not carotid disease. LV function is actually more than 30%, they do not have LV thrombus.
Dr. Oussama Wazni: Valvular?
Dr. Walid Saliba: They do not have valvular heart disease. So there is still a large patient population who are at an increased risk of stroke, who do not fit necessarily the WATCHMAN criteria. So how much do we extrapolate and how many patients do we include just by clinical practice is something that real time data is going to be able to tell us [intangible].
Dr. Oussama Wazni: It seems to me that we may need a randomized study of WATCHMAN versus the new oral anticoagulants at some point.
Dr. Walid Saliba: So I think that it's very important to think now about a WATCHMAN in two different environments. One is where is the place of the WATCHMAN in the arena of newer anticoagulant? And more importantly, where is the place of the WATCHMAN with the growing atrial fibrillation ablation population?
Dr. Oussama Wazni: Any final thoughts on this therapy?
Dr. Walid Saliba: We are very excited about the availability of this therapy. I think it is definitely a practice-changing therapy and it gives us a lot of room for future research. There's going to be a lot of newer devices that are going to be on the market that we're also going to be involved in evaluating and I think the future is bright and exciting to see how things are going to lead us.
Dr. Oussama Wazni: In my practice, I have to say the patients are very, very comfortable with the therapy and very satisfied with it. I mean, they come back and thank me for their improvement in quality of life because now they don't have to worry about taking an anticoagulant that may cause bleeding and repeated visits to the emergency department. So I think it's a new era in stroke prevention and I think it gives us a lot of new options to treat those very high risk patients, whether it's ischemic stroke, or with bleeding. And at that, I thank you very much for joining me Walid, on this-
Dr. Walid Saliba: Thank you, it's a pleasure.
Dr. Oussama Wazni: ... podcast and thank you very much.
Dr. Walid Saliba: Thank you.
Announcer: Thank you for listening. We hope you enjoyed the podcast. We welcome your comments and feedback. Please contact us at heart@ccf.org. Like what you heard? Please subscribe and share the link on iTunes.

Love Your Heart
A Cleveland Clinic podcast to help you learn more about heart and vascular disease and conditions affecting your chest. We explore prevention, diagnostic tests, medical and surgical treatments, new innovations and more.


