Aortic Aneurysms
December 1, 2020
Having an aneurysm can be a scary diagnosis. Vascular surgeon Dr. Sean Lyden and vascular medicine specialist Dr. Scott Cameron answer many questions patients have about aortic aneurysm:
- What is an aneurysm?
- Who is at risk for aneurysm?
- Where do aneurysms occur in the body?
- Can aneurysms be managed medically?
- When should an aneurysm be fixed?
- Can aneurysm disease be genetic?
- What kind of screening tests should patients have for aneurysm?
- Are there symptoms?
Learn more about the Cleveland Clinic Aorta Center
Subscribe: Apple Podcasts | Buzzsprout | Spotify
Aortic Aneurysms
Podcast Transcript
Announcer:Welcome to Love Your Heart, brought to you by Cleveland Clinic Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute. This podcast will help you learn more about your heart, thoracic and vascular systems, ways to stay healthy, and information about diseases and treatment options. Enjoy.
Dr. Sean Lyden:
Welcome, everybody. My name's Sean Lyden, I'm the current chairman of vascular surgery at the Cleveland Clinic, and joining me today is my colleague Scott Cameron, who is the new head of vascular medicine at the Cleveland Clinic. We're just going to talk a little bit today about aneurysm disease, because it's generally a topic that can be very terrifying to patients. Depending on where it is, there's a lot we can actually relay. Scott, why don't you start off with maybe a comment or two about aneurysm patients, like who gets them, who we need to look for in them, and how we find them?
Dr. Scott Cameron:
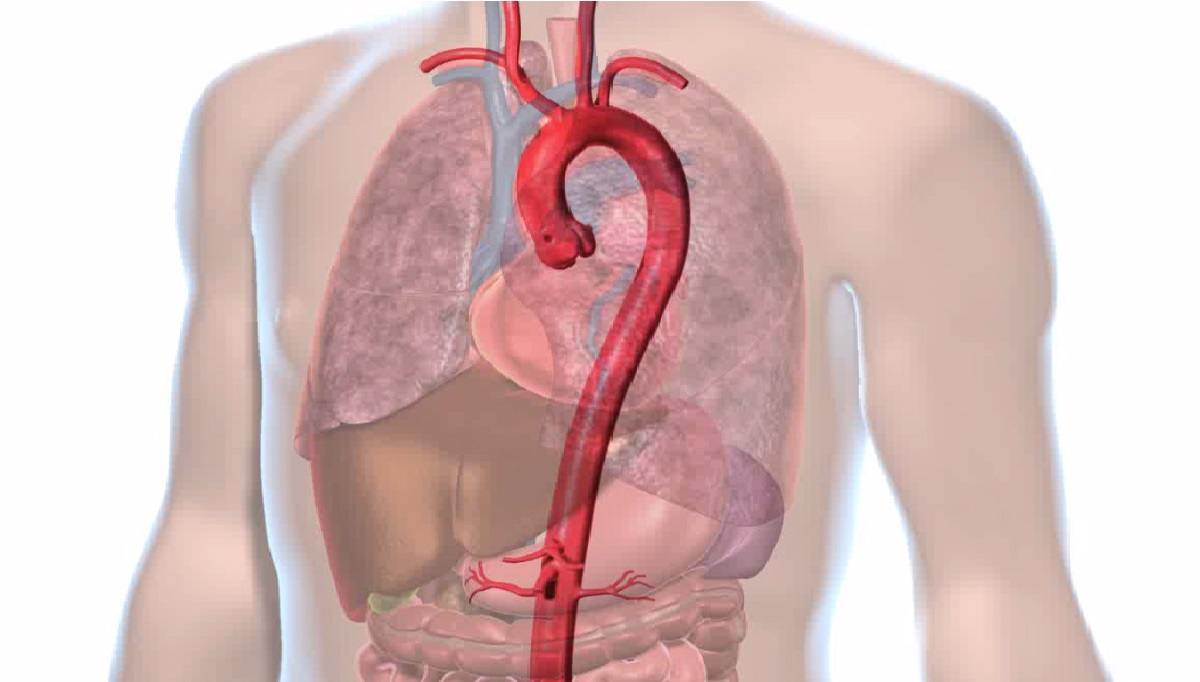
Sure, thanks, Dr. Lyden. So I typically find that patients that present with aneurysms, they can be in any blood vessel, but quite often it's the aorta, one of the main blood vessels going through the body. Truthfully, in my practice, a lot of them are found incidentally. They've had an imaging scan for some reason that's not related to the blood vessel, and then the question naturally becomes, well, what do I do with this information? What is the growth trajectory of this aneurysm based on the size? Is there a medical treatment for it, or, in fact, do I need surgery?
Dr. Scott Cameron:
Those are excellent questions, and I think that they can cause undue anxiety for good reasons in patients. Certainly reading certain things on the internet can make one a little bit concerned, so in the Heart, Vascular & Thoracic Institute, physicians like myself who are trained in vascular medicine and cardiology, and surgeons like Dr. Lyden really work in a multi-disciplinary manner. We have a real time of experts and we basically collectively make the decisions that are best for the patient, including screening and medical management.
Dr. Sean Lyden:
I think that's a great point. When we look at aortic aneurysms, they can happen in several places in the body. They can happen in the ascending aorta, where really they'll be evaluating whether or not the heart valves are involved, and that would be a decision joint between the cardiac surgeons and the cardiologist, but in the thoracic aorta ... just to the left arm artery or in the chest, interesting enough, they generally have a genetic predisposition, so many times we'll send those patients for genetic counseling to figure out is there a genetic predisposition in their families?
Dr. Sean Lyden:
Those aneurysms tend to happen about equally in men and women, and then when we get to the abdominal aorta, it has a very male determination, four times more common in men than women. But all these are really related to smoking, so maybe, Scott, you want to comment on when see a patient with the aneurysm disease, besides the aneurysm and whether it should be treated or not, what are the other things we try and take the opportunity to address in terms of lowering their risk and improving their overall longevity?
Dr. Scott Cameron:
Yeah, that's a really important question, Dr. Lyden. One of the things that I find is that, just as you said, the aneurysms that people have in the aorta or the area below the diaphragm, there's three groups of people, and overwhelmingly, in my practice, I find that they're atherosclerotic. So patient have an underlying hardening of the arteries, remodeling of the arteries, and if you see that in the aorta and it's been enough to cause an aneurysm, what I typically find is that there's another blood vessel bed, another vascular bed, that has the same issue. In my practice, it tends to be the heart.
Dr. Scott Cameron:
One of the things that we quite often see is that patients that have an aneurysm in the aorta also have some disease in the arteries and the heart, the coronary arteries, and they're not aware of that. Sometimes we see that patients have got disease in blood vessels in the brain, or the blood vessels going to the brain, the carotid artery, as I'm sure you also see in your practice.
Dr. Scott Cameron:
So the question then begins, if it's atherosclerosis and hardening, certain smoking is a risk factor. But the other risk factors that I often see and quite often spend a lot of time treating is I find that the patients have high blood pressure, just as you find in clinic. When the pressure's high inside the blood vessel that may have a region of the wall that's slightly weak, it stands to reason that that might be something that could accelerate the aneurysm, the growth of the aneurysm.
Dr. Scott Cameron:
So I take control of blood pressure extremely seriously, and certainly in the medical phase, before a patient requires surgery, those are things that we can manage not only just by in-visit encounters, we can also manage by virtual visits. We're doing a lot more of them in the COVID-19 era, unfortunately, but I'd say that those patients that have issues with high blood pressure, we can serve quite well even with virtual consultations. It doesn't always require an in-person consultation.
Dr. Sean Lyden:
I think that's a great point, Dr. Cameron. I think the key thing is, as you pointed out earlier, most of these are incidental findings. You may have had back pain or abdominal pain or a cough, you get an ultrasound or a CAT scan that reveals this, and the first thing is, when people hear they have an aneurysm, it's very scary. Really, I try and explain to people what an aneurysm is. Every blood vessel has a normal size, and if it gets 50% larger than normal, we call it an aneurysm. Really, we try and individualize when you need it fixed. It's really, what is the risk of that aneurysm, and then what is the risk of the treatment?
Dr. Sean Lyden:
There are societal guidelines based on whether there's valve disease, the size of the aneurysm, in terms of how often it needs checked and when it should undergo treatment. I think one of the key things is that we've seen in the last decade a growth of the minimally invasive or catheter-based treatments to treat these aneurysms, and we've led a large number of trials here at the clinic to develop those technologies and really to push them forward so that at least half the patients we see, all the way from the heart valve all the way down to their groin, have options of an endovascular treatment and do very well with really less invasiveness, a quicker recovery with really the same longevity.
Dr. Sean Lyden:
But I think the question people always ask me is, well, what do I need to tell my kids? Why did I get this? Maybe, Dr. Cameron, you can talk about some of the gaps we have in our knowledge. What are the things that we're working on together to help better understand who gets these aneurysms and how we can predict whether they grow fast or need treated sooner?
Dr. Scott Cameron:
That's a really interesting question. It's a natural question for somebody who has children or somebody who has brother and sisters: what is the likelihood that there's a heritable component to it? Now, there are certainly some aneurysms, in fact, I saw a patient with this last week, that had an aortic aneurysm, but based on a very careful physical exam, which is something we do recommend for the first visit, you can sometimes be given clues on the exam that it might not be caused by hardening of the arteries or risk factors, but there may be something wrong with the structural proteins within the blood vessel wall.
Dr. Scott Cameron:
In the case of this patient recently, we diagnosed with Loeys-Dietz syndrome, which is extraordinarily rare. Loeys-Dietz syndrome is a heritable disorder, we do know a little bit about the genetics, and we're really fortunate at the Cleveland Clinic that we can really build on the armamentarium of clinical geneticists, clinical counselors, genetic counselors, as well as physicians and surgeons. In this particular case, I did recommend that this patient have their child screened, and it turns out that the child also had Loeys-Dietz syndrome and has since become a patient of mine. So that's a classic example of just a clue in the physical exam and just now paying attention to an image, you can sometimes pick up other things in the patient.
Dr. Scott Cameron:
Now, one thing that Dr. Lyden and I have certainly been working on in the last year is trying to figure out, is there a blood test or some kind of marker that's not an imaging study that might tell us, just by a blood sample, is this a patient that we can tell might have a fast-growing aneurysm or a slow-growing aneurysm? That's the one thing that I would say that patients tend to worry about.
Dr. Scott Cameron:
Well, it turns out that there are actually a couple of markers that we've found, and we've started to enroll patients, we've actually enrolled 212 patients in the last 12 months, and we're using those samples, which are blood draws at the same time as routine clinical care. It's free, it's not part of the patient's medical record, but it's allowing us to learn and actually develop what could be one of the first blood tests to predict this is how fast an aneurysm would grow.
Dr. Scott Cameron:
And that certainly gives us a little bit of a heads-up, because I'm sure, Dr. Lyden, you must've been in the situation at this point in your career, where an aneurysm's growing faster than what we might've predicted, and the patient then presents at the time with a dissection, or even worse, a rupture, which is a bona fide surgical emergency. I wonder if you could maybe tell us some of the things that we could do as physicians and that we continue to do to prevent that from happening.
Dr. Sean Lyden:
I think the first thing is awareness. As you pointed out, patients always say, should I be concerned? Why should I be concerned? So if you've had a first degree of relative, a brother, a sister, a mother or father, a child with an aneurysm, you probably should get checked. If it's an aneurysm in the chest, it's a 50% chance it might be spread to you. If it's in the abdominal aorta, it's maybe only 15%.
Dr. Sean Lyden:
But I think the other thing is, once you know you have it, engaging in routine follow-up, making sure it's not growing faster, and then as Dr. Cameron pointed out, controlling those risk factors. I think that's one of the things we really try and stress here is getting people to stop smoking, to control their blood pressure; those are directly correlates with how fast the aneurysms grow, the risk of rupture. And really, when people know about it, and if it were to have a dissection or rupture, it's a lot easier to treat if you've had some prior imaging.
Dr. Sean Lyden:
There's nothing tougher than, you know, a patient has their first presentation and it's a rupture and the aneurysm is eight, nine centimeters and may have existed in the patient for three to five years before anybody knew about it when it presented with a catastrophic problem. I think that awareness is something we're pretty proud of. Just yesterday, Governor DeWine in Ohio signed a bill that's starting ever February 13th, it'll be Aortic Awareness Day; in September, there's an Aortic Awareness Week, and I think the key thing is just having that awareness.
Dr. Sean Lyden:
If you're older than 65 and you're a man and you've smoked, you're welcome to a Medicare physical, we'll get an abdominal aneurysm screening. But if you have a family history, generally most insurance companies will cover when the physician documents you have risk. So maybe, any other closing thoughts in terms of things for ... common questions we get asked for our patients and our families when they come see us with these problems?
Dr. Scott Cameron:
A question that I get asked quite a lot, Dr. Lyden, I'd be interested to hear your perspective, if patients ask this in the surgeons' office, is if I have an aneurysm that may be small or large, but it's about to become weaker and might develop a tear or a dissection, or the worst-case scenario is it develops a rupture, where the blood vessel can actually split, what would that feel like? One of the things that I've told patients, because I've seen this in my practice: patients sometimes present with abdominal pain, they sometimes present with back pain.
Dr. Scott Cameron:
But having taken care of, oh, I don't know how many patients with heart attacks, I tell them that with a dissection or a rupture, it's very different. It usually comes on like that, just all of a sudden, and your body knows. You might not know what it is, but you know what your body feels. And if you have an aneurysm, that would be a go-to-the-emergency-room kind of situation. It's not like heart pain, heart pain, if there's not enough blood supply getting to the heart, almost reproducibly, in most patients, what I find is that if they exert themselves, the symptoms will get worse. If they rest, the symptoms get better.
Dr. Scott Cameron:
I find that the patients that I've seen with aortic dissection and rupture, it comes on abruptly. But what I will also tell you, I have seen patients present in the emergency room even with findings on the electrocardiogram that can make it look like a heart attack, but it actually was an aortic rupture.
Dr. Scott Cameron:
So one of the things I always encourage patients to do if they know that they have an aneurysm, even if it's being tracked, is that if they can make sure that they know where their closest hospital is, we're fortunate, as I'm sure you'll attest to, this is a center of excellence, we're used to seeing very complicated case and we're used to handling them. But just sort of knowing what they might do if they feel those symptoms come on abruptly. I'm not sure if you have a similar thing that you might tell patients in clinic.
Dr. Sean Lyden:
Yeah, when we see patients with aneurysms, especially for an abdominal aneurysm, we say it can present with severe abdominal pain or back pain. A lot of the patients who we see with this are older than 65, they may have some spine disease, they may have some other chronic abdominal aches and pains, and they say, well, how will I know this is my aneurysm as opposed to I've had some diverticulitis and some inflammatory disorder in my colon, or I have a bad back?
Dr. Sean Lyden:
I think the one thing I uniformly say is that this will feel very different than any pain you've ever had. As Dr. Cameron brought on, it's a very abrupt onset, it's very severe. I would uniformly say that patients, it'll be different than the usual pains they get, in terms of having a bad back or some chronic abdominal pain, and it's not one of those where you're sitting around saying, oh, is that my aneurysm? Maybe I should go to the ER today.
Dr. Sean Lyden:
I reassure patients that when they have normal aches and pains, those are normal aches and pains. When you have pain when your aneurysm is either dissecting or rupturing, it is much, much more intense. Any time we've had a patient have that happen, they all describe that it was completely worse, completely different, and there was no question in their mind that this was something I had to go to the ER.
Dr. Sean Lyden:
I reassure them that the normal aches and pains are not a problem, and that once their aneurysm is at a size where the risk of that aneurysms exceeds the risk of us repairing it, that we will want to guide them through the best way to repair it, whether it's a traditional open surgery or a minimally invasive repair, and make sure that that repair lasts for a lifetime.
Dr. Sean Lyden:
I think the thing we know here is we have very, very good outcomes, and the fact that we take care of this a team approach and really assess what other cardiovascular issues they have, whether it's heart disease or cerebrovascular disease, because the biggest thing outside of the aneurysm rupturing that really leads to death of our patients is heart attack and stroke and really blood pressure control and smoking cessation, are the two things that actually help with that. And then you add upon that cholesterol control, and it's really key for all these patients, including all of our patients with aneurysms.
Dr. Scott Cameron:
Yeah. Dr. Lyden, I wonder if I could ask you, just in general terms, a patient or two that might stick in your memory as to this is a classical story where you should make patients aware of aneurysms. One I just thought of was a gentleman who I had treated for heart disease for a number of years, and he had a little bit of peripheral vascular disease, his blood pressure was well-controlled, and it suddenly occurred to me at his clinic visit ... I had a mixed practice then, cardiology and vascular medicine; now, as you know, I almost exclusively focus on vascular medicine, since I'm most passionate about that.
Dr. Scott Cameron:
It occurred to me this patient was 66, and it occurred to me that I had been completely unable to get him to stop smoking, no matter what I did. So I mentioned to him, you know, you're 66, active smoker, and you're welcome to Medicare packages, as you said, you have a one-time screen, he had no symptoms, his physical exam was normal. So I did the screening ultrasound in his abdomen and got a call from the lab, he had a 7.6-centimeter dissecting aneurysm with a luminal thrombus.
Dr. Scott Cameron:
And the one thing that I took away from that was the screening guidelines are there for a reason, so if you know particularly if you're a male and you've smoked and you're 65 or older, you should get screened. But the second thing I took away from it was this was quite different from the heart attack he'd had previously. He just stopped smoking. He had failed every pharmacological therapy we had tried, he just didn't want to do it. And his question to me was, what made you look? And I said, well, there's a guideline for it and that's why we looked.
Dr. Scott Cameron:
He said to me, after I found out I had that in there, this thing brewing, he said it was enough, I never went back to cigarettes again. He just kind of always stuck with me as one of a more dramatic case where he didn't have any symptoms. I wonder if you've had any patients like that. Dr. Lyden.
Dr. Sean Lyden:
I literally just had an experience, literally in the last two weeks. We've worked with pretty much all the companies that helped bring many of the current devices on the market to trial, and one of the former marketing managers for one of the medical device companies called me and said her grandfather had a fall and had a CAT scan and found a very large eight and a half-centimeter aneurysm.
Dr. Sean Lyden:
She never really thought to think that maybe someone in her family would have this disease process that ... she worked for a company that was developing these devices, and really just the a-ha that grandfather had smoked his whole life, he was now in his 80s; he was otherwise perfectly healthy, and if he hadn't had this fall, this large aneurysm would not have been found, and would've more than likely been his cause of death at eight and a half centimeters. That had about a 30% chance per year risked, it was fixed, he had his heart evaluated and had it fixed in Florida two days later.
Dr. Sean Lyden:
But just really, she called me from the work we did helping to get their devices approved, saying wow, it really never dawned on me that I might have, my own family member had this. Even though she'd been to events and we've talked about there's free screening and that it could be paid for, she never really thought to go home and say, well, hey, how about my dad and my grandfather? After she let me know her grandfather did well, I said, well, Dad's above 65, he needs to go get his test now too, and so does all the brothers and sister.
Dr. Sean Lyden:
I think you really have those sort of a-ha moments where they're just found incidentally and you really continue to do well, and the sort of really ... the bad moments are when you have a patient who might've been told about it, but then forgot or didn't seek follow-up, and they had something that may have been really treated well with very little risk as an elective fashion that presents ruptured and you're unable to save them.
Dr. Sean Lyden:
I had a patient about six months ago who had been told he had an aneurysm and decided it didn't need addressed and sort of forgot about it until it presented ruptured. We got him all the way to the OR here and just couldn't get him through it because the degree of shock from the bleeding. So the key is thinking about it, getting it looked at and getting it treated before it's a really big problem.
Dr. Sean Lyden:
So with that, I really want to thank those people who have watched this. At the clinic, we really ourselves of really working together collaboratively between the vascular medicine department, the vascular surgery department, and we hope that you look at our resources on the web if you have questions in the future, or come see us someday.
Announcer
Thank you for listening. We hope you enjoyed the podcast. We welcome your comments and feedback; please contact us at heart@ccf.org. Like what you heard? Subscribe wherever you get your podcasts or listen at ClevelandClinic.org/loveyourheartpodcast.

Love Your Heart
A Cleveland Clinic podcast to help you learn more about heart and vascular disease and conditions affecting your chest. We explore prevention, diagnostic tests, medical and surgical treatments, new innovations and more.


