Calcium, Bone Density and Osteoporosis with Drs. Pelin Batur and Chad Deal
Subscribe: Apple Podcasts | Spotify
Calcium, Bone Density and Osteoporosis with Drs. Pelin Batur and Chad Deal
Podcast Transcript
Nada Youssef: Hi, thank you for joining us. I'm your host, Nada Youssef, and today we're talking about osteoporosis. Osteoporosis weakens bones, making them susceptible to sudden unexpected fractures. The disease often progresses without any symptoms or pain, and is not found until bones fracture. Today we will talk to our Cleveland Clinic experts regarding steps you can take to prevent this disease and treatments that may be needed.
Here with us today, we have two experts. We have associate professor of medicine for the Ob Gyn and Women's Health Institute, Dr. Pelin Batur, glad to have you. We also have with us head of the Center for Osteoporosis and Metabolic Bone Disease and Rheumatologists, Dr. Chad Deal.
Dr. Pelin Batur: Thank you.
Nada Youssef: Nice having you as well. I want to start, first of all with Dr. Batur. I want to explain to myself and to the audience why we need a woman's health aspect to this, why it's important that you're here?
Dr. Pelin Batur: Yeah, hormonal treatments can be very, very helpful for bone. Because obviously for most patients with osteoporosis, is going to be postmenopausal women who have lost estrogen. Hormone therapy, which we'll talk about it a little bit more, there's a better understanding of risk versus benefits, and there was a scare many years ago that it's a lot of risk and not much benefit.
Now we really understand that depending on the woman, you can really get a lot of benefits from hormones, bone health being one of them. Sometimes we use hormonal treatments to minimize the duration of use of our other bone agents. So we really worked closely together between women's health and the osteoporosis center, to help treat our patients.
Nada Youssef: Sure. Excellent, thank you. And for our viewers, whoever's watching, you can leave your questions in the comment section below. If you have any questions, we'll ask them live here. Before we begin, please remember, this is for informational purposes only and it's not intended to replace your own physician's advice. All right, so let's start, Dr. Deal, with explaining what is osteoporosis?
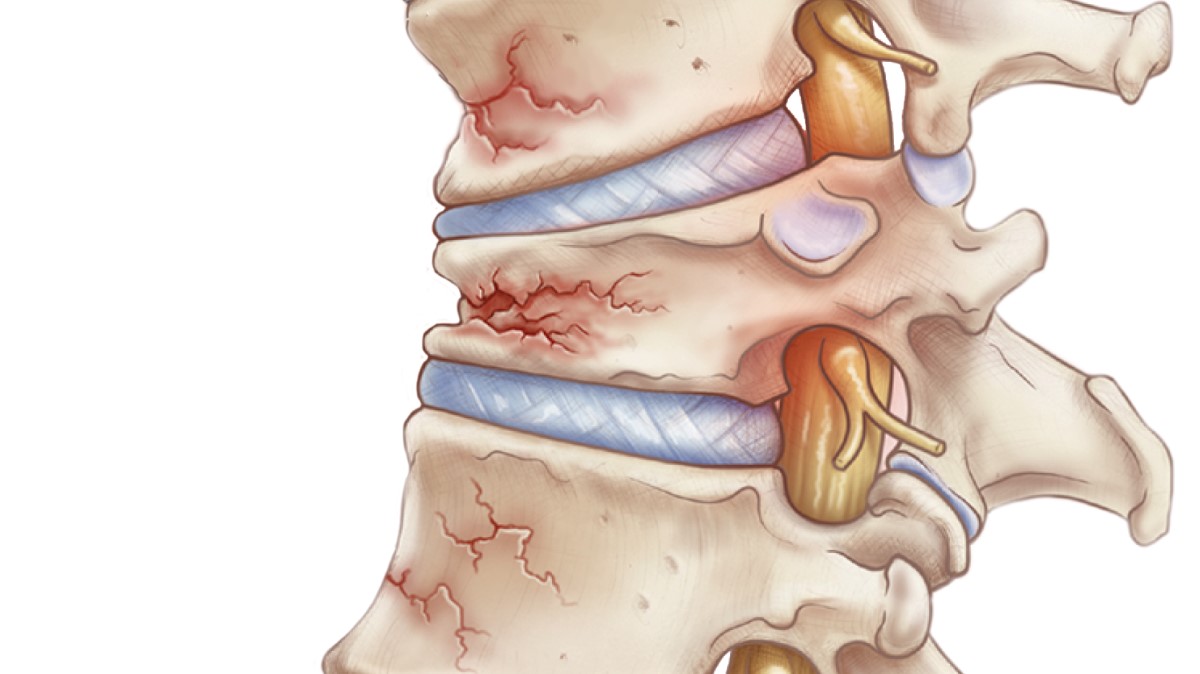
Dr. Chad Deal: So most people know osteoporosis as a disease that causes fractures. Prior to that though, for a very long time, you can have osteoporosis and not even know it. It's basically what we call a micro architectural deterioration of bones. So, think of a skyscraper as it goes up with all these girders, and as time goes on in your bone, you're missing a few of those girders which creates weakness. The weakness gradually accumulates until you have a fracture.
So it's really important for both men and women to get a test for osteoporosis prior to the fracture, because in most cases we can actually prevent the fracture if we know that the patient has either Osteopenia, which is a little bit not quite as bad as osteoporosis, in advance and use some of the drugs. Whether it's hormone replacement, or bisphosphonate therapy, or many of the other drugs that we have.
Nada Youssef: Okay. So before a fracture ever happens, are there any symptoms that the patients may be feeling and that knowing that could be osteoporosis.
Dr. Chad Deal: Right, and that's why we've called it the silent thief. People generally, they don't have any symptoms until a fracture occurs. So that's very different than, for instance, osteoarthritis. Where if you have it in your knee, you're going to have stiffness and swelling, as an early warning sign that the joint is deteriorating. But with osteoporosis, no, you have no symptoms.
Nada Youssef: All right. And then, who is at risk? I know women are definitely at risk, and it's called also a woman's disease, correct? Some people refer to it.
Dr. Pelin Batur: There's a lot of men that are underdiagnosed, so it's not just a woman's disease, but it is most common in women after menopause. We're really looking at anybody who's lost their sex steroids, so that would be estrogen for women and testosterone for men. Also patients who have been thin throughout their life, which we define as less than 127 pounds; that's a risk factor. Certain medical conditions, diabetes, rheumatoid arthritis, will increase risk.
Those who've had a previous fracture are at a risk for another fracture. We also look closely at the medication list. For example, women who've had chemotherapy, for example, for breast cancer, and are now taking anti-estrogen treatments. People who are taking steroids. Those would all be things that we look at, at the med list to see if they're on a medication that can increase the risk.
Nada Youssef: Is Age a big factor as well?
Dr. Pelin Batur: Age is one of the biggest factors.
Nada Youssef: Okay. Why is that?
Dr. Pelin Batur: If we look at any bone density, and let's say somebody has a bone density test in the osteopenia range, not quite osteoporosis, and they are 50 years old, their risk of fracture is going to be much lower as opposed to somebody with that same bone density who is now 65. So in fact for each five years that passes after age 65, you're essentially doubling your risk of fracture. So age is one of the biggest things that we worry about for fractures.
Nada Youssef: Okay. Then, so the cause is unknown. But how does that disease develop?
Dr. Chad Deal: Well, we do know a lot of the causes for low bone mass for osteoporosis. About 70% of peak bone mass is genetically determined. So by the time you're 25 or 30, 70% of your bone mass is done. That's why it's really important to have a healthy lifestyle as a youth, that includes not smoking, and low alcohol intake, and lots of exercise and normal body weight. But there are environmental issues as Dr. Batur has already mentioned, that affect peak bone mass.
A lot of the times it's known, but the genetics of it are very complex. There are at least 100 genes or more that control peak bone mass, bone loss. So you might think of genes that control vitamin D metabolism, or calcium absorption, or osteoblast function, these are the cells that produce new bone. Or osteoclasts, the cells that break down bone. So there are lots of genes involved that we don't understand.
Nada Youssef: Sure, sure. Are there certain diseases or medical conditions that contribute to bone loss more than others?
Dr. Chad Deal: Yeah. So the reason I'm here, I'm a rheumatologist. I got interested in this because many of my diseases can result in bone loss. One would be rheumatoid arthritis. In fact, rheumatoid arthritis is a risk factor. If you go to this FRAX website, if you just google in FRAX on your computer, you can calculate your 10 year risk of a fracture, and rheumatoid arthritis is one of the risk factors. In addition, for all the inflammatory diseases that rheumatologists treat with steroids, that's a huge risk factor. So we're talking about cortisone, prednisone, those types of medications. They're very big risk factors. But it's not only rheumatology, all subspecialties use steroids or prednisone as part of their treatments for various inflammatory diseases.
Nada Youssef: Right. The medications can also, there are some medications that can cause some bone loss?
Dr. Chad Deal: Well, I think Dr. Batur also already mentioned aromatase inhibitors in women with breast cancer. Those are antiandrogen therapy. For men is antiestrogen, antiandrogen therapy in men with prostate cancer for instance, that's a big risk factor. But there are others like seizure medication, Dilantin, that accelerate vitamin D metabolism and can cause low bone mass. So there are lots of medications that can do this, can accelerate the process.
Nada Youssef: Sure. Okay, and now let's switch onto the dietary factors, and you talked about that a little bit, even when by the age 25 or earlier you should be healthy. Let's talk about diet, is there dietary factors that can contribute to this disease.
Dr. Pelin Batur: I'm glad you're asking me this question, because I'm going to keep rewinding this for my kids.
Nada Youssef: Good, good. That's important.
Dr. Pelin Batur: Just like you said, by 20, 30 we're building up something that's important. I mean what you're doing throughout your youth and with your lifestyle, it really makes a big difference. So we want to make sure that patients are getting enough calcium. We prefer dietary calcium as opposed to supplements whenever possible. Realize that, that's not always possible. We have patients you know who have gastrointestinal issues or lactose intolerance, they may not be able to get an adequate dairy calcium. Dairy is your best way of getting calcium. There's other ways, but if you're lactose intolerant it's going to be hard for you to get that.
So getting enough calcium is probably one of the most important things. And truth be told, nobody knows exactly how much calcium is required. There's some controversy with that, but we think somewhere around 1000, 1200 milligrams a day. I see people who are either getting way too little calcium or sometimes getting way too much, because that amount of the 1000 to 1200 should be everything, including supplements and what's in your diet.
Nada Youssef: Okay. So they could be too much calcium.
Dr. Pelin Batur: Mm-hmm (affirmative).
Nada Youssef: That can also cause bone loss.
Dr. Pelin Batur: It won't cause bone loss, but adding extra calcium is never going to help you to your bone. Either you're going to pee it out or there's some concern about whether it leeches out into the arteries. Calcium is a safe supplement overall, but just like anything else, you want everything to be in moderation, too much of anything isn't good. Plus it's constipating, at least most types of calcium.
Nada Youssef: Right. What about lifestyle choice?
Dr. Chad Deal: Lifestyle includes exercise, you're talking about things like that. So the good example of exercise would be as if you go into space, you lose about one to two percent of your lumbar spine bone density every month, so that's total weightlessness. Obviously that's not something that our audience is going to experience. But, if you're a couch potato, you can lose bone mass not to that extent too. Weight bearing activity is really important, and when I say weight bearing, I'm not talking about lifting weights, we're talking about heel strike. So putting your foot to the floor and sending a mechanical stimulus through your skeleton.
We have cells in our body called osteocytes that are mechanoreceptors, and they take that vibration and they turn it into something that stimulates osteoblast to produce new bones. That kind of lifestyle's really important. I think we've already mentioned calcium. We've already mentioned smoking-
Nada Youssef: Smoking and drinking.
Dr. Chad Deal: ... alcohol. Alcohol is a direct toxin to osteoblasts. The kind of the cut point for that for men is about three drinks a day, 21 a week; it may be less for women, more toxic to the cells. Smoking, nicotine is really bad for your bone. There's nothing. Nicotine is good for everything, including the bone.
Nada Youssef: Sure, sure, and even those guys in space have treadmills and they have certain things to do to keep their bones strong, right?
Dr. Chad Deal: Yeah, they do.
Nada Youssef: Because they lose a lot of bone mass.
Dr. Chad Deal: The Cleveland Clinic was involved in a project, try to do what we call counteract the effects of weightlessness so that we can go to Mars. In order to do that, you've got to do some kind of weight bearing activity going to Mars and back. Otherwise, you're in real trouble, and so that's an experiment that's still ongoing at NASA in Johnson city, but it started at The Cleveland Clinic.
Nada Youssef: Wow. That's amazing, I didn't know that.
Dr. Pelin Batur: I think it's important to emphasize it's not just about taking a supplement, or getting half an hour of working out in a day. It's really about lifestyle. Eating nutritious foods, taking good care of yourself, and I do see people who are taking a bunch of supplements, but they go on these fad diets, and they lose a bunch of weight that ... of course we want you to be a healthy weight, but they do it through eliminating of a lot of wholesome foods. And then I see a huge decline in their bone density, the year after. There's a lot to be said for just taking plain old good care of yourself.
Nada Youssef: It's kind of reversible, you can fix ... If your bones are starting to be weak, you can fix it with your lifestyle and dietary choices.
Dr. Pelin Batur: Yeah, to a certain extent. Sure.
Nada Youssef: Okay. Well, we talked about how there is no signs or symptoms for osteoporosis. But, I know you mentioned earlier there a test that people should take. What age, who should take it, and what test are we talking about?
Dr. Chad Deal: Okay, my guideline is a little bit different than the official guideline. The official guideline is every woman at age 65 should have a bone density test. But if you have clinical risk factors for bone loss, so that would be low body weight, or smoking, or family history, or previous fracture it really should be at menopause. Because so many women enter menopause with low bone mass already, and there's a subset of women that can lose up to five percent of their bone mass every year for six years.
You can lose a third of your bone mass and a six year period. The only way to really attack that is to know if you need to treat it right away, and a bone density test is the best way to do that. For men, the guideline is age 70, unless there's risk factors, and in which case we do edit age 50.
Nada Youssef: Okay. We're talking about a bone density, right?
Dr. Chad Deal: Yeah, and it's a $100 test. It's part of a welcome to Medicare, so when you go get your medicare insurance, that's part of the test that's covered by Medicare. But, most commercial insurance will pay for it if you have risk factors. I think it's a test that's well worth $100, even if you had to pay for it yourself in order to maintain skeletal integrity and prevent fractures.
Nada Youssef: Can you describe to the audience, walk through what kind of a test ... what does that look like? What to expect going into a bone density test?
Dr. Chad Deal: Yeah, it's really easy. It takes about five or 10 minutes. You lie on a table and there's a x-ray beam that sends a x-ray through your skeleton, the hip and the spine, and the amount of x-ray that gets through the bone and is detected on the other side is proportional to the amount of calcium in the bone. When I say x-ray, remember this is a very low x-ray procedure. It's about one-tenth of the amount of x-ray of a chest x-ray. It's about the same amount of radiation you get flying from Cleveland to San Francisco. So it's not something you should worry about in terms of x-ray exposure.
Nada Youssef: Okay, good. That was going to be my next question. Okay. Let's jump onto treatments. I want to talk to you about treatments, what treatments there are. And I know for women it's probably different for man. So we'll kind of tag team and talk about that.
Dr. Pelin Batur: Yeah, we have lots of treatments available. We have hormonal treatments, which technically hormone replacement therapy for the younger woman is meant to be for preventing osteoporosis and fractures. But we do have great data, many, many years of data that suggests that actually it helps prevent fractures. And hip fractures which is important, because not all medications available have been shown to prevent hip fractures, which is one of the types of fractures that we really worry about.
Because that's the one that can really impact ... affect disability in terms of putting you into a nursing home. Or increasing your chance of having a bad outcome and increasing death. That's where a hormone therapy can be very helpful, especially for the younger woman who's got pretty severe bone loss. But we have many, many non-hormonal options available. We have what we call. also designer hormones.
So these are called selective estrogen receptor modulators, SERMs. Or sometimes people call them estrogen receptor agonists antagonists. But really what the name is trying to define is, that it works like an estrogen in some body parts, and as an anti-estrogen in other body parts. So for example, the one that we have approved for bone health is an anti-estrogen at the breast. So it's also used for breast cancer prevention.
I would define it as a little bit of a weaker bone medication, so probably a perfect ideal candidate for that one would be a younger woman that has significant bone loss, and she has a family history of breast cancer. She wants to prevent that risk, but her risk of fracture right now isn't that high because she's still younger.
What you can do is you can kind of insert that therapy for five years or so, so you kind of postpone when she's going to switch over to another therapy. And I'm sure we'll talk about that. There's bisphosphonates, these are the bone medications that come in pill form, injectable form, oftentimes just taken once a week or once a month. Then we have also a bone builders and other injectables.
Nada Youssef: Great. Would you be taking the same approach? I know you're more of a-
Dr. Chad Deal: Yeah, absolutely. Yeah. The bone builders, what Dr. Batur was mentioning are anabolics. So we divide therapy into anabolic or bone building, and anti-resorptive. The anti-resorptives prevent bone resorption, or bone breakdown. Those include estrogens and the SERMs that were mentioned along with the bisphosphonates.
The bone builders, we have two of them now. We have Forteo and Tymlos, and they're both PTH analogs, PTH being parathyroid hormone. They're injections and they're expensive, but for patients at high risk for fracture who've already had fracture, who have very low T-score, they're our go to drug for the severe osteoporosis case. I think they're underutilized, and should be considered in patients with severe osteoporosis.
Nada Youssef: Sure. Now-
Dr. Chad Deal: Yeah, I was going to say for the bisphosphonate medications you may have been asked, were going to ask me that. There's a real fear of using these medications now. The two things that people think about as side effects are these atypical fractures or this brittle bone, and osteonecrosis of the jaw. I always tell my patients there's no free lunch, there's always a risk to everything you do. You could take an aspirin tablet, swallow and it could stick on your esophagus and you could burn a hole in your esophagus if you don't do it properly.
Our job as osteoporosis specialist is to treat people at high risk for fracture so that the benefit of the drug outweighs the risks. Now, having said that, atypical fracture risk is with these drugs. These are thigh bone or hip fractures that occur spontaneously with long-term therapy. They don't really occur in the first three years of bisphosphonate therapy. They are issues related to long-term therapy. For that reason, we have guidelines now for drug holidays with Bisphosphonates.
Nada Youssef: Drug holidays?
Dr. Chad Deal: People with mild or moderate risk might be on the drug for three to five years, and then they get time off for good behavior. But it's not really time off, because these drugs, the bisphosphonate medications, bind to bone. They stayed there a long time, so I call it administrative holiday, but the drug's still actually working. That's not true for estrogen. That's not true for SERMs. That's not true for anabolics. Once you stop those, the effect goes away very rapidly.
Dr. Pelin Batur: Then we also have, another injectable called Prolia. That's actually helpful for our patients who have kidney dysfunction. Patients with weakly functioning kidneys oftentimes can't tolerate some of the other bisphosphonate medications, and the injection done like a flu shot, essentially; getting it twice a year at the doctor's office, and tends to be well tolerated.
So the point is we really have a lot of options, and we use all of these medications regularly. It's about the individual person, what's in their medical background, what are their priorities, what are they feel comfortable with, and we take it from there. And oftentimes we will change the medication that we're using over time. So the long-term medication, the side effects that you were mentioning, the osteonecrosis of the jaw, the unhealed wounds of the jaw and the femoral neck fractures, these seem to be an issue with longer term use.
So oftentimes if it's a younger woman, we can use something hormonal for five to 10 years. Then we know that when we take her off the hormones, that bone density is going to drop. Now she's in her sixties and maybe she doesn't need the hormones anymore, because she's not having any hot flashes. Then we can step in with our other bone agents. That way we're minimizing the duration of use. So we're maximizing the benefit, but minimizing some of those long-term risks.
Nada Youssef: Very good. And we're getting a lot of questions. We'll get to them here in a second. But first, Dr. Deal, I Want to talk about osteoporosis in men. Is the common? Or is it more common than we think?
Dr. Chad Deal: More common than you think. About 20% of all hip fractures are men.
Nada Youssef: 20%.
Dr. Chad Deal: Yeah. So it's a small, but substantial group. So there are two differences with men from women, or maybe more. But one is men have higher peak bone mass, so about 10% more peak bone mass, so that means that they fractured later in life if they do fracture. The second thing is they don't have abrupt decline in hormones like women do at the menopause. Testosterone decline as much more gradual over time, so that tends to protect them from fractures, but not totally. As I mentioned, 20% of all hip fractures are men, and the same risk factors that we've talked about already for women apply to men. So healthy lifestyle, calcium, vitamin D intake, smoking, alcohol, they all apply to men.
Nada Youssef: I don't think we touched on this. There are primary and secondary osteoporosis? Can you explain these two main types and what causes second osteoporosis in men?
Dr. Chad Deal: That's a kind of a nomenclature term. Primary is when there's no appearance. Secondary cause, like rheumatoid arthritis, or steroid use, or vitamin D deficiency. Those are mostly just the genetics of it. The secondary causes are those that we can identify a definite reason for the osteoporosis, and hopefully intervene and do something about it.
Nada Youssef: Okay. And then the risks don't differ for men. Correct? The risks are both for women and men the same.
Dr. Chad Deal: Yeah. There's almost total overlap in risk factors for osteoporosis between men and women.
Nada Youssef: Okay, great. Thank you guys. Well, I'm going to go ahead and head to some live questions that we're getting. I have Brandon, "A daily dairy calcium source versus nondairy calcium source, which is better?"
Dr. Pelin Batur: As long as you're getting your calcium as through a natural food source, that's okay. I don't think one is necessarily better than the other. I usually give a printout of how much calcium is in different foods, and you can actually find that on our Cleveland Clinic website because I oversee a lot of the women's health, Cleveland Clinic patient education materials for the hospital.
So if you Google Cleveland Clinic Patient Education, you'll have a whole bone section that goes into vitamin D and calcium, and we try to update those every few years so that they're up to date with accurate information. I think it's important for everybody just to add up their typical average day calcium intake. You can do that with fancy Google calculators or apps, or you could just do simple arithmetic, and just see. Because on our website, it lists different types of foods and how much calcium per serving.
One thing to keep in mind some of the green leafy vegetables, sometimes our body has a harder time extracting the calcium from those. So I always tell people, don't overestimate, be accurate. If you're saying, "Oh, that looks like about a half a cup of Kale," don't say that's half a cup of Kale. I would really look at your intake, because you might not be getting quite as much calcium from some of the green leafys.
Nada Youssef: Great.
Dr. Pelin Batur: Oh, and then the one other thing-
Dr. Chad Deal: So, that was Brandon, right?
Nada Youssef: Yes.
Dr. Chad Deal: That asked that?
Nada Youssef: Yes.
Dr. Chad Deal: He may be getting at whether, if you go to a website, vegan website, there's lots of information about calcium from dairy versus nondairy source. So there's a fair amount of controversy. I think that Dr Batur and I agree that food calcium from any source is probably good, but there is controversy in that area.
Dr. Pelin Batur: I think one important thing to bring up is that, your body typically can only absorb about 500 milligrams of calcium at one time. So what I see a lot of times it's somebody who sat down with their fortified cereal, had their fortified orange juice, put their milk-
Nada Youssef: And cheese.
Dr. Pelin Batur: ... took their multivitamin. They said, I'm done for the day. No, your body's very smart, smarter than us. It controls how much calcium is going to absorb. It's one thing if you're trying to make sure that you're getting the right amount of calcium intake, break that up throughout the day. Don't take a supplement when you already took a multivitamin, because you're probably going to just pop that out.
Nada Youssef: Yeah. Great. Then Shirley, "What are things you can do if you already have osteoporosis as a result of Crohn's and other health issues?"
Dr. Chad Deal: Well, Crohn's disease, there are a couple of reasons that people with Crohn's have low bone mass. One is, many of those folks with inflammatory bowel disease have been on steroids or prednisone, which can cause bone loss. Second reason is that, especially if they've had surgery, they may have malabsorption and they may not absorb calcium and vitamin D very well at all.
Many patients might have low body weight, and that's another risk factor. When you talk about therapy for those folks, you've got to address all those issues, and correct to the extent you can all those issues. If they still have low bone mass, then that's where you step in and use one of the active drugs that we have to either prevent bone loss or buildup bone.
Nada Youssef: Sure, sure. Now, I wanted to ask you, where do you go for that bone density exam test? Do you go to your primary care physician? Do you need to see a specialist?
Dr. Chad Deal: Well, so bone density machines used to be more prevalent, and they used to be in many, many primary care offices. But over the last decade or so, reimbursement for bone density has declined rapidly and many bone density machines in private offices have gone away. So often they're in hospital based radiology departments, but there's still a very significant number in private offices.
The machines cost about 50, 60, 70 thousand dollars. They're not too expensive, but they're not too cheap. It's fairly easy to find one.
Nada Youssef: Okay, great. Thank you.
Dr. Pelin Batur: It's helpful to make sure that you're getting your bone density on the same machine. So that, in two years when you're following up on that, exactly. So you can compare change. Because it's like otherwise, getting on a scale and trying to determine one or two pounds difference on different scales.
Both Dr. Deal and I read thousands of scans per year, so at our institution we take great pride in making sure that we're all certified, and that we're following the international society guidelines. You want to make sure that you're getting it from a professional place, and following up on the results there.
Nada Youssef: Great. Thank you. Chris. "For women who have been diagnosed with breast cancer and are taking estrogen blockers, what are the natural therapies that they can use to prevent their bones from thinning?"
Dr. Pelin Batur: So I'm assuming when they say natural, Chris, you said, was thinking about supplements.
Nada Youssef: I guess so, yeah.
Dr. Pelin Batur: So let me address that first, because I get that question a lot. In terms of soy supplements. That's one of the most common questions that we get. Soy can have estrogen like properties, and so our oncologists get a little nervous about the use in supplement form. Because when we look at plant estrogen, even though it's found in nature, it's completely unnatural to our body chemistry. We don't have estrogen that looks like that.
On our website that I mentioned the calcium sheet, it also talks about the hormone therapies. There we talk about different amounts of soy, how much estrogen they have. So if you're doing it naturally through diet, I think that's okay, but when you're doing it in supplement form, I get a little nervous.
People also take strontium sometimes as a supplement. The recommendation is to not use that. People use fluoride. In fact, if you're just looking at bone density data, fluoride is probably going to help improve your bone density more than many other products that we have. But why don't we use it, it probably increases the risk of fractures. The medications that we recommend have been really tested, and we're looking at outcomes like fracture data.
The problem with some the supplements that, although they're labeled as natural, we don't really have the safety data.
Nada Youssef: FDA.
Dr. Pelin Batur: Right. Yeah. So, I mean, I recommend supplements in my practice, but I'm a little nervous in terms of osteoporosis health, bone health. Outside of the calcium and vitamin D, we don't have data about safety or effectiveness of the others.
Nada Youssef: Right. So it's okay to eat soy in your diet, but not, supplements probably stay away from.
Dr. Pelin Batur: Right, and as long as you're not overdoing it. Again, some of our oncologists do it, because depending on the type of breast cancer treatment you're receiving, some, like Tamoxifen for example, work by really competing for that estrogen receptor. So, if you're getting a little extra estrogen from a lot of soy, it's probably okay. But for medications like aromatase inhibitors, which function by really dropping that estrogen level, the oncologist really worried about any kind of estrogens seeping into the system, that it may actually make it not work as well.
Nada Youssef: All right. And then I have a Gloria. "I have osteoporosis. What can I take to relieve stiffness and pain, as I am on Warfarin?"
Dr. Chad Deal: She doesn't have stiffness and pain from the osteoporosis as we mentioned, it's silent. So her stiffness and pain is probably related to degenerative joint disease, or I'm not sure where the stiffness and pain is. That's a different issue for stiffness and pain. Other than physical therapy, and stretching, and heat and all the non-medicine type of therapies, we often use nonsteroidal anti-inflammatory drugs for stiffness and pain, but that's really not related to osteoporosis.
Nada Youssef: And that's why it's called silent bone thief, right?
Dr. Chad Deal: Correct.
Nada Youssef: Because you never know what's happening.
Dr. Chad Deal: Correct.
Dr. Pelin Batur: Well, I think the big source of confusion is because they both have the term "osteoporosis" in it, which means bone, but osteoporosis literally means porous bones, so it's weaker. Osteoarthritis, which causes a lot of the pain means inflammation.
Nada Youssef: Okay, great. Then Bonnie, "I'm a kidney transplant patient and on prednisone and work out and walk a lot. What else can I do to stop the pain?" More pain questions.
Dr. Chad Deal: More pain.
Nada Youssef: Wow, we have a few.
Dr. Chad Deal: Well, I don't know why she has pain so that's a hard one to answer. Sorry.
Dr. Pelin Batur: Yeah, it needs an evaluation probably with rheumatology.
Nada Youssef: Okay, great. So I'm going to go ahead and see here we got Lydia, "What are the pros and cons of," tell me if I'm doing this right. Is it Reclast infusion?
Dr. Pelin Batur: Reclast infusion.
Dr. Chad Deal: Yeah.
Nada Youssef: "Reclast infusion?"
Dr. Pelin Batur: So the Reclast is one of the bisphosphonates that we mentioned. Well tolerated, we have great data on the effectiveness. It's given once a year, and we use it for at least three to five years and then do a bone holiday for most people, unless it's severe. Really, there's not many contraindications, so that one of the reasons we wouldn't use it if somebody had significant kidney dysfunction, we'd be hesitant about that.
But one of the nice thing about the injections is that we're guaranteeing that it's being absorbed. So when a patient takes an oral pill, like for example, if they take oral Fosamax, roughly about one one-thousandth of that is absorbed. So if they're not taking it properly on an empty stomach, they're drinking it with their coffee, absorption might be an issue. Or if somebody has bowel issues that prevent absorption, so at least we're bypassing all that and we're ensuring that it's absorbed.
Also, if somebody does have issues with reflux esophagitis type of symptoms from the pills, then the IV formulation helps bypass that.
Nada Youssef: Okay.
Dr. Chad Deal: It's a simple an infusion. It takes about 20 minutes, you do have to have an IV. About 10% of patients get a post infusion reaction. We call it flu-like, it's not the flu. But they may have low grade aches and pains, low grade fever for 24 to 48 hours.
Nada Youssef: And that's 10% of ...
Dr. Chad Deal: Yeah. It's a Medicare B drug, so it's covered very well by Medicare. The out of pocket expenses are usually very small. It actually went generic a few years ago when the price, for instance of that drug is like $350 for an infusion once a year, so it's really actually very cost-effective medication.
Nada Youssef: Great.
Dr. Pelin Batur: They're actually using at oncology too, some of these medications and bisphosphonates, to prevent metastasis to the bone. So there's probably some other health benefits that need to be more studied.
Nada Youssef: Okay. I have another question about another medicine. Allison wants to know, "What are the pros and cons of Prolia?"
Dr. Chad Deal: Right, and I think Dr. Batur mentioned Prolia. Prolia, so we've talked about bisphosphonates that are chemicals and they bind to bone. When an osteoclast comes along the bone surface to resorb the bone, the bisphosphonate's taken up in the osteoclast function is inhibited.
Prolia or Denosumab is completely different. It is a monoclonal antibody against rank ligand. Rank ligand is a cytokine that's absolutely essential for osteoclast function. Osteoclasts being the cells that resorb bone. It's a shot given every six months. When you stop this drug, the effect goes away very rapidly. So we're not talking about drug holidays with this drug.
It's a very effective drug. We actually have a 10 year study now, in 2,500 people showing its safety over a 10 year period. It does have some of the same side effects as the bisphosphonates, including rarely these atypical femur fractures or osteonecrosis of the jaw.
I should say something about ONJ osteonecrosis of the jaw. 90% of patients who get that tend to be the cancer patients, who are getting the high dose medications, Dr. Batur mentioned. They have cancer, they tend to get Reclast or Prolia in super high doses. 10 times the osteoporosis dose. About five to ten percent of these ONJ cases are in osteoporosis patients.
But in most cases these are patients who have dental procedures that involve exposed bone like a tooth extraction or very poor dental hygiene. For that reason, when we're starting one of these drugs on a patient, and they have some dental issues, we always like them to get those dental issues cleaned up and taken care of before we start the medication.
Nada Youssef: Sure.
Dr. Pelin Batur: One more plug in for the hormonal therapies. The hormone therapies in the SERMs that I mentioned, they have not been linked to some of these long-term risks such as of the jaw and if the femoral neck. For women who are appropriate candidates or are suffering with a lot of menopausal symptoms, they can't sleep, vaginal dryness, I mean a whole menopause complex mood concerns; this is a way that you can avoid the long-term use of one medication.
Nada Youssef: Right.
Dr. Chad Deal: Yeah, and the anabolic drugs, the bone builders Forteo and Tymlos, they're not associated with atypical fractures or ONJ either.
Nada Youssef: Wow. All right. And then we're having questions about Fosamax. Terry wants to know, "Are there natural treatments without taking drugs such as Fosamax?"
Dr. Pelin Batur: Similar to what we've talked about before, there's really no natural supplement that we know that works. If we lived in a country where there was more strict regulation of the supplement market, I would feel so much more comfortable. But we're seeing increased number of liver transplants from supplements. Because, you can make a lot of claims on supplements. Because everybody wants to be healthy and there's people with money in their pockets. So it's a business model built on very little oversight by any federal FDA-
Nada Youssef: Yeah.
Dr. Pelin Batur: Exactly. There's people out there to make a buck, and they may have the best intentions of putting out a pure product, but there's issues with impurities. They found rat poison, chemotherapy agents, in some of the supplements. Without the data to show that there's any supplement that helps, I'm a little nervous about recommending it.
Nada Youssef: Supplements, you don't need a prescription for. You could just go get it from wherever, or online, right?
Dr. Chad Deal: Yeah.
Nada Youssef: Yeah, that's just great.
Dr. Chad Deal: Some people, they ask me, "Can I do this with just calcium and vitamin D alone," for instance. What I usually tell folks is that, we have randomized controlled trials that led to the approval of all the drugs we've talked about today. The placebo group is calcium and vitamin D, so we know that when you add an active medication to calcium and vitamin D that you reduce your risk for fracture.
Calcium and vitamin D are important, and when you are on one of these medications, you still need calcium because calcium is the building block of bone. Fosamax is not calcium. You still need the calcium.
Nada Youssef: Sure.
Dr. Pelin Batur: It's kind of a quirky analogy. I mean it's not perfect, but I liked the way it feels in my head. I think of calcium and vitamin D as a bunch of bricks, and I think of the medications that we're recommending when the bone diseases really bad as like a bricklayer. When you have a wall that's falling apart and the bricks need to be put together, dumping more calcium and vitamin D, so dumping more bricks isn't going to fix the problem.
And having a bunch of bricks and no bricklayer isn't going to help. Or having the bricklayer, which is the mediation without the adequate number of bricks, the calcium and vitamin D, isn't going to help. So it's that delicate balance of both that you need.
Nada Youssef: Yeah. That makes sense. Joanne wants to know if Fosamax causes jaw pain?
Dr. Chad Deal: Well, jaw pain. First of all, there are lots of reasons for jaw pain. We have patients who walk into clinic and they've stopped their Fosamax because they have clicking and their jaw, and that's TMJ, that has nothing to do with OMJ. There are many reasons for jaw pain. Muscular pain, grinding your teeth at night. Everything that that causes pain in the jaw or the face is not related to Fosamax.
Osteonecrosis of the jaw, there's a definition for it. It's exposed bone that persists for more than six weeks. So if you look in your mouth, you'll see an area where the gums gone and where you can see exposed bone and that persists. That's ONJ the rest of the causes for pain in the jaw are something else.
Nada Youssef: Okay.
Dr. Pelin Batur: Thank you for asking that, because that comes up a lot. And let's not forget ONJ and the atypical femoral fractures actually occur and people not on these medications.
Nada Youssef: Oh, okay.
Dr. Pelin Batur: So this is not just from these medications. So in fact, if you look at hip fractures, it turns out a good number of them can be these atypical fractures, and people not on meds. We're just concerned that it may slightly increase the risk, but these slightly increased risks that we're talking about are in the rare category. One out of a thousand or less.
Nada Youssef: Oh wow. All right, great. Then Darlene wants to know, "Should I take vitamin D or D3, and what is the difference?"
Dr. Chad Deal: D2 or D3? Sorry.
Nada Youssef: Vitamin D or D3.
Dr. Chad Deal: So there's two types of D. There's D2, and that's usually the prescription that we write. It's 50 thousand unit D2. It's plant based. D3 is over the counter. So that's where you get 400, 1000, 2000, 5000, you can just pick it up off the shelf. That's an animal source product, okay? D3 may be a little more potent than D2, not a huge difference. So either is fine.
Nada Youssef: So, D3's the animal, you said?
Dr. Chad Deal: Uh-huh, and D2's the vegetable.
Nada Youssef: Okay.
Dr. Pelin Batur: Consistency is the key.
Nada Youssef: Consistency.
Dr. Pelin Batur: The nice thing about vitamin D is fat soluble, so it's one of the only vitamins that you can take more in lump sum. I always tell people if you forgot it for a week and you say, "Oops," then you can actually double up the next week, and it's similar to taking it every day. You shouldn't do that with other vitamins, but vitamin D is one that's reasonably safe. As long as you're sticking to the lower over the counter doses, and not a high prescription dose.
Nada Youssef: I'll follow up with Cathy's question. She wants to talk about high dosage vitamin D, is it safe, and do you need to take calcium with it?
Dr. Pelin Batur: Vitamin D, you ask 20 different people, you're going to get 60 different answers. Back in the day when we really didn't have as much data on vitamin D, I would use the higher dose in my practice, the 50,000 units. I still have to in some women that have had, for example, bariatric surgery and have really hard time absorbing. But I favor finding a lower dose of it that you can take regularly. That way I can see.
Because I've seen some people accidentally take ... we use the 50,000 units, sometimes one to two times a week. But I've seen people accidentally taking it once a day. I think there's some predisposition, yeah, to error with that. I really tried to find what's the minimum that the patient can use, and usually I don't recheck levels for about three, four months to get a real idea of the plateau. Your approach may be different.
Dr. Chad Deal: No, I agree with that. We tend to use the 50,000 in patients who really have very low vitamin D's, because we want to replete them very quickly. Because people who have really severe vitamin D deficiency can have, not osteoporosis, but osteomalacia. Osteomalacia is a failure of bone mineralization, and vitamin D is really required for that.
The typical patient would be patient who's had bowel surgery, and they have what we call short bowel syndrome. They come in and they have a vitamin D level of five, normal being 30. Those folks have a lot of unmineralized bone. They have something we call osteoid in the bone. Those patients need very quick repletion of vitamin D, in order to get their bone mineralized. That's where we tend to use the bigger pills that Dr. Batur was talking about, the 50,000.
Nada Youssef: Sure.
Dr. Pelin Batur: We should probably talk about, the optimal level of vitamin D, because that's also an area of confusion. So the National Institute of Medicine Guidelines say anything over 20 is adequate. But really with bone health ... that's for general population. But for patients who are having a lot of achiness, or those with osteoporosis, many of us would feel that, that's sub-optimal. We try to strive for over 30, ideally 40 to 50.
I'm a little nervous about too much vitamin D. Again, since it's fat soluble, you may not be able to pee it all out and you can get toxic on it. So although we have data on safety at the higher ranges, even more than 100, in surfers and people who are out in the sun getting it naturally, we don't have that safety data for supplements. I try to stick to somewhere between 30 and 80, mostly before 40 to 50 range really.
Nada Youssef: Great.
Dr. Pelin Batur: I don't know if your approach is different.
Dr. Chad Deal: Yeah, I mean, the normal's 30 to 80.
Nada Youssef: 30 to 80.
Dr. Chad Deal: As I said, there is controversy about whether you need 20, whether you need 30 nanograms per deciliter. But most folks in the osteoporosis go with 30 nanograms or greater.
Nada Youssef: Okay. Great. Then, Agnes wants to know, "I'm on a weekly medication for osteopenia/osteoporosis. I follow the rule on an empty stomach and do not lie down or drank my coffee for 30 minutes to one hour. How beneficial is the injection over the pills?"
Dr. Chad Deal: So, she's asking whether taking the injection, which would be Prolia or the infusion, which would be Reclast, might be better than Fosamax. Now if you take your Fosamax properly as she's doing, empty stomach, big glass of water, don't have anything to eat or drink for at least 30, maybe even longer, it's going to be effective therapy.
Where I think where you get some improvement with either Prolia or Reclast are in patients who are not quite as compliant with their oral medicines, or forget their oral medicines or take it with a cup of coffee as Dr Batur mentioned earlier. In those cases the injection or the infusion may be a better choice.
Nada Youssef: Okay. Great. Then Gwendolyn, "What can you do about constipation due to calcium supplements?"
Dr. Pelin Batur: Yes, that's a good question. Sometimes just fixing the behaviors that worsen constipation is helpful. So what do I mean? Really pushing the fluids, especially when the weather starts to turn. People don't realize that they're getting relatively dehydrated, because the heaters are kicking in. So I really encourage patients who are constipated, to really aim for six to eight glasses of water a day. Minimizing other agents that are constipating.
You always want to make sure that thyroid has been checked, and you don't have another reason to be constipated. Benefiber, I don't want to advertise certain supplements. But a fiber form, Benefiber is one of our favorites in our clinic. Just staying regular with that. There's some data that calcium phosphate might be a little bit better in terms of constipation. Personally I've seen that to be true.
It's harder to find, but you can find that in some gummies. Used to be able to find it as Posture-D, but I think they got rid of that a while ago. I've seen it at Sam's and Costco it's chewables.
Dr. Chad Deal: All right, so calcium, that brings up the point of calcium, supplements come in. Calcium carbonate, calcium citrate, calcium phosphate, calcium gluconate. Most patients, the most common on the market is calcium carbonate, so that's what's in Tums or Oscal or Caltrate. Citrical, I find a little bit less constipating too.
The advantage of taking calcium citrate is, it's absorbed independent of acid. You don't have to take it with a meal, you can use it in patients who have a disease called pernicious anemia where they have no stomach acid. It's absorbed very well too. The disadvantage of the Citrical is the elemental calcium is less, so you have to take a bigger pill and more pills often with Citrical than you do with calcium carbonate.
Dr. Pelin Batur: It's a little bit more expensive, too. I'm glad he mentioned about the acid because, keep in mind that if you're on medications to block stomach acid, like your Prilosec, your Nexium which a lot of people are on, then you really should stick to something like the calcium citrate as opposed to the calcium carbonates, because you're not going to absorb the calcium carbonate as well.
Nada Youssef: Sure. Okay. Well, I'm going to give you one more question before I let you guys go. Lynn wants to know, "What things caused me to have a higher chance of getting osteoporosis?" I'll kind of end up with that, we can talk about. Because we've talked about that earlier, lifestyle, choices, dietary. Then also, I want to kind of touch on pain because I feel like a lot of people were asking about pain management with this. So we want to kind of clarify everything here, as a kind of our conclusion for today.
Dr. Pelin Batur: I think one thing I'll touch on for this question that we haven't touched on, is women with premature menopause. Those would be defined as before age 40. These women have accelerated, not just bone aging, but heart aging and brain aging. So these women really should be on hormone therapy, unless there's a reason not to be, until about age 50 to 51, 52, the natural ages of menopause so that we really don't create osteoporosis 20 years before they were meant to.
We oftentimes do that even if a woman went through menopause at age 43, a little earlier, but not the definition of premature menopause. Unless she has a compelling reason not to be, she usually will feel better and she'll protect her bones.
Nada Youssef: Mm-hmm (affirmative). Great.
Dr. Pelin Batur: Yeah, and you ask about pain. As we already have mentioned, this is a silent disease until you have a fracture. There are some folks who have vertebral fractures or spine fractures, and they have a tremendous amount of pain. In many cases that pain will resolve over six or 12 weeks. But in some cases it may not. There's a procedure called kyphoplasty where they actually insert a cement type substance in the vertebral body, and that sometimes helps resolve pain.
Sometimes patients who have chronic pain end up in medical spine centers, and places that deal with chronic pain in the spine. Another common cause of pain with a fracture are sacral fractures or pelvic fractures, they can be very painful. We do our best to treat them, as we do many other pain patients.
Nada Youssef: Sure. Well, thank you both so much for taking time educating us in the audience, and thank you for watching. We hope you enjoyed today's discussion.
To download our free osteoporosis guide, and learn more about prevention, treatment options, please go to Cleveland Clinic.org/osteoporosis. For more health news and information, make sure you're following us on Facebook, Twitter, Instagram, and Snapchat @ClevelandClinic, just one word. We'll see you again next time. Thank you.

Health Essentials
Tune in for practical health advice from Cleveland Clinic experts. What's really the healthiest diet for you? How can you safely recover after a heart attack? Can you boost your immune system?
Cleveland Clinic is a nonprofit, multispecialty academic medical center that's recognized in the U.S. and throughout the world for its expertise and care. Our experts offer trusted advice on health, wellness and nutrition for the whole family.
Our podcasts are for informational purposes only and should not be relied upon as medical advice. They are not designed to replace a physician's medical assessment and medical judgment. Always consult first with your physician about anything related to your personal health.


