A colectomy (colon resection surgery) is treatment for conditions like colon cancer or severe inflammatory bowel disease (IBD). A colectomy may remove specific parts of your colon, all of it, or your colon and your rectum.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
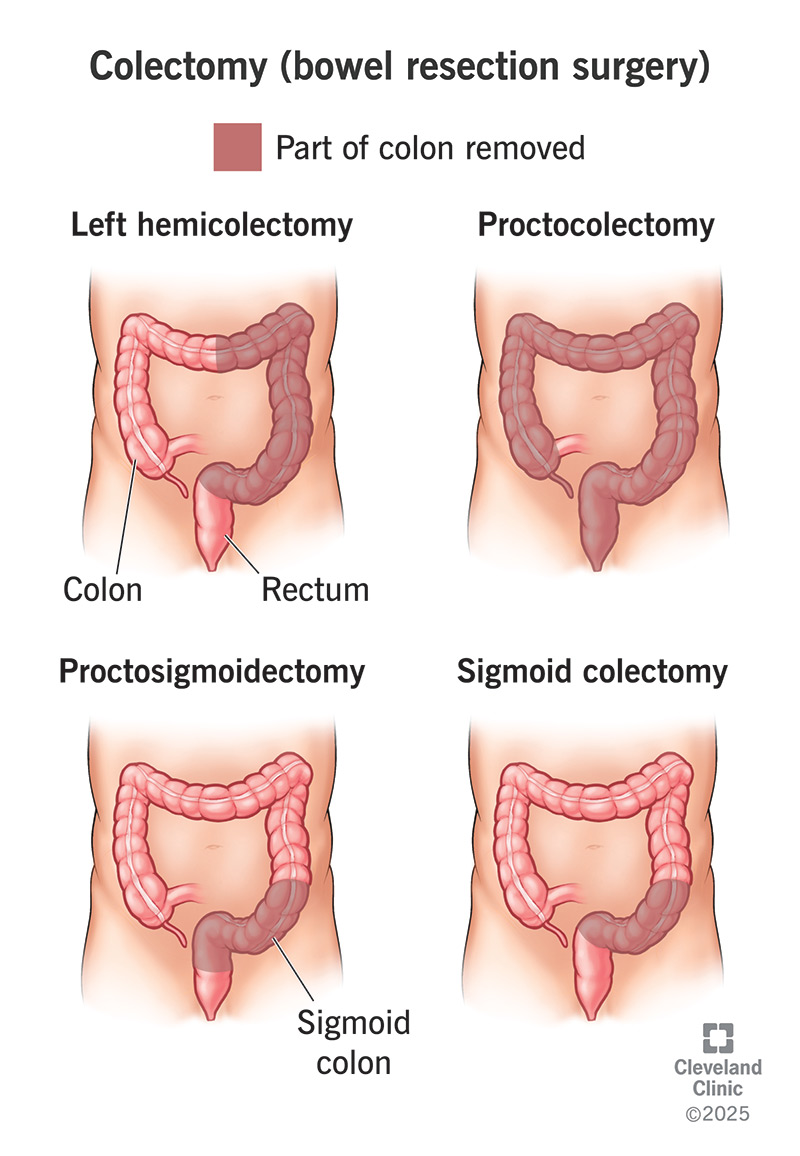
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4671-colectomy.jpg)
A colectomy is surgery to remove part or all of your colon in your large intestine. You may have a colectomy if you have a condition that damages your colon. The damage may affect your gastrointestinal tract so it can’t work like it should.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Healthcare providers may do colectomies to treat the following conditions:
There are inherited disorders, like Lynch syndrome, that increase colon cancer risk. Familial adenomatous polyposis (FAP) is another example. If you have these conditions, a preventive colectomy may reduce your risk.
A total colectomy removes your entire colon. A partial colectomy removes certain sections of your colon. There are different types of partial colectomies:
A colectomy is major surgery. There’s a lot that goes into preparing for it. First, you’ll meet with your gastrointestinal surgeon. They’ll discuss the specific type of colectomy you’ll have and the method they’ll use.
Your healthcare team will do tests to confirm you’re able to have surgery. You may have tests like:
Advertisement
They’ll also explain what you should do during the few days before your surgery. General guidelines are:
Here’s what happens during a colectomy:
A colectomy may take between one and four hours to complete.
Having a colectomy may change the way poop leaves your body. Normally, digested food moves through your colon on its way to becoming poop. Removing part or all of your colon can disrupt that process.
Surgery to remove damaged sections of your colon divides it into two sections. Your surgeon may be able to connect the two sections (anastomosis). This lets poop continue to move through your colon.
But sometimes, that’s not possible. In that case, your surgeon will do an ostomy as part of your colectomy surgery.
Like all major surgeries, colectomies may cause complications. Potential complications include:
You’ll stay in the hospital for a few days up to a week. Your intestines can’t process food right after surgery, so you’ll be on a liquid or soft diet for few days. Your healthcare team will check the surgery site for any issues.
Your team will explain how to care for your incision. If you have an ostomy, your care team will explain how to care for it and how to adjust to life with an ostomy bag.
They’ll also explain what you can eat as your intestines recover from surgery. They may have suggestions for activities that you can do once you get home, like walking.
This is a lot of information to take in at any time, especially when you’re just starting to recover from surgery. You may want to have a family member or friend sit in on these conversations.
Recovery at home may take up to six weeks. Many people get back to most of their usual routines within two weeks after surgery. But your recovery time may be different. Try to be extra gentle with yourself. Resist the urge to race back to your routine.
Advertisement
In general, you should stick to low-fiber foods for the first month after surgery. Low-fiber foods are easier for your colon to process.
Contact your surgeon if you have:
A colectomy is treatment for several conditions. Some of them, like colon cancer, can have an impact on how long you live. Other conditions, like diverticulitis, cause painful symptoms but aren’t life-threatening. And colectomy may be just one part of your treatment. You’re unique, and your life expectancy may be different from that of other people. Ask your healthcare provider about life expectancy. They know you and your situation. They’re your best source of accurate information.
A colectomy surgery may be a life-changing experience. The surgery may ease painful gut symptoms, be a potential cure or help you to live longer with colon cancer. In some cases, the surgery may mean having an ostomy that creates a new way for poop to move out of your body. You may worry the ostomy will affect your lifestyle. Your healthcare providers will understand this may be a big adjustment for you. They’ll be glad to answer your questions. They’ll recommend resources for managing changes a colectomy surgery may bring.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Some conditions like rectal and colon cancer, Crohn’s disease and ulcerative colitis may require colorectal surgery. Cleveland Clinic has the expert care you need.
