Hartmann’s procedure is a type of colectomy that removes part of the colon and sometimes rectum (proctosigmoidectomy). The remaining rectum is sealed, creating what is known as Hartmann’s pouch. The remaining colon is redirected to a colostomy. It can be reversed later.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
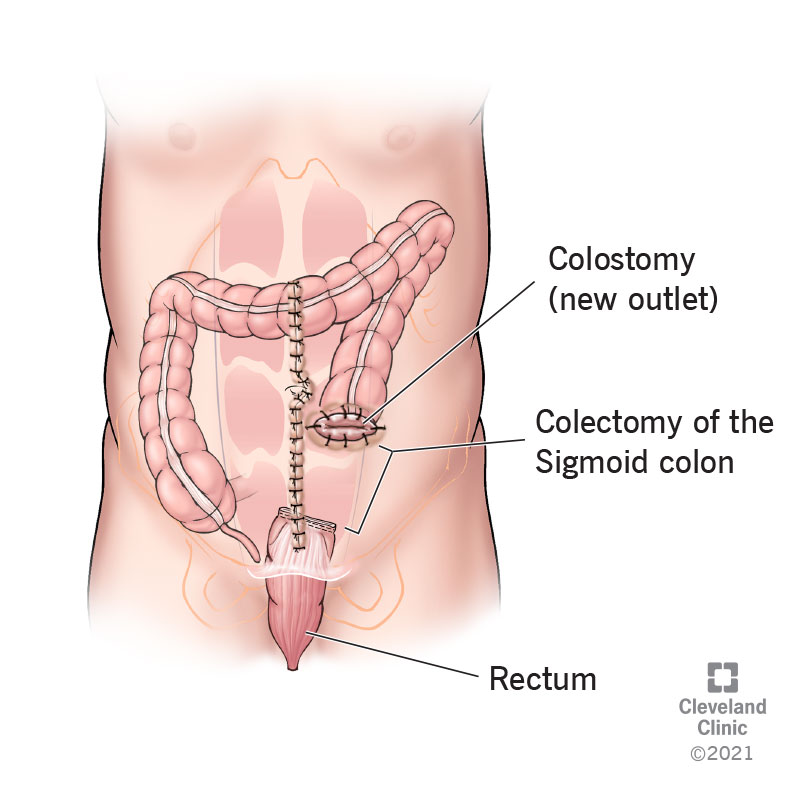
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21891-hartmanns-procedure-illustration-final.ashx)
Hartmann’s procedure, also called proctosigmoidectomy, is a surgical operation on the large intestine (colon). It’s a specific kind of colectomy, which means that part of the colon is removed. Hartmann’s procedure removes the last part of the colon, called the sigmoid colon, where it joins the rectum — and sometimes part of the rectum too. This is the end of food’s journey through the digestive tract, where it is almost ready to be expelled as poop. Hartmann’s procedure interrupts and redirects that journey.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hartmann’s procedure is often an emergency operation to remove an obstruction, persistent infection or cancer before it can spread. When a portion of the bowel is removed under these conditions, the remaining portions can’t be safely reattached at that time. Infection, inflammation and other factors make it too technically difficult or too dangerous to attempt rejoining the sections in the same surgery. The colon needs time to heal. So, Hartmann’s procedure seals the remaining part of the rectum and diverts the remaining part of the colon to a new outlet, called a colostomy.
The surgeon will make a new opening in your abdomen and attach the remaining colon there on the inside. They'll give you a colostomy bag to attach to the outside of the opening. This is where your poop will come out. Hartmann’s procedure is often a life-saving intervention, and it involves a significant life change. But it’s not always permanent. After your colon has had a chance to heal, your surgeon will reevaluate your condition. If they find you fit for additional surgery, they can perform a reversal about 6-12 months after the first procedure, rejoining the colon to the rectum and closing the colostomy.
There are two parts to Hartmann’s procedure. First, it removes a portion of the lower bowel. Second, it redirects the remaining bowel to a colostomy. There are different reasons for these two parts.
Advertisement
Any part of the colon may need to be removed if:
Removing the unhealthy part of the colon saves the healthy part and allows the rest of your digestive tract to continue to function as normally as possible.
When surgeons remove part of the bowel and reconnect the remaining ends during the same surgery, it’s called “resection with primary anastomosis." This longer and riskier surgery is possible when you are in good overall condition and there isn’t a risk of infection or inflammation in your remaining bowel. Hartmann’s procedure treats those at higher risk and whose condition may be more complicated. The colostomy allows the surgeon to focus on solving the immediate problem at hand while leaving open the option to reverse the operation at a more appropriate time.
When discussing Hartmann’s procedure, doctors sometimes refer to the closed-off part of the rectum and anus as Hartmann’s pouch. (This is different from Hartmann’s pouch in the gallbladder.) Because the rectum side is sealed and the anus side is open, and the leftover length is relatively short, it’s like a pouch. It doesn’t have any special function, but doctors might discuss it as a separate part of the body to watch for infection or disease, especially if you’re having the procedure to treat diverticulitis or cancer.
The surgery is most commonly performed for:
Other, less common reasons include:
Hartmann’s procedure may be performed through laparoscopic surgery or open surgery, depending on your condition. Traditional open surgery involves opening up the abdominal cavity to access the organs. Laparoscopic surgery is a newer method that uses smaller incisions aided by a tiny camera called a laparoscope. The laparoscopic method is less invasive and involves less recovery time, but it isn’t always possible to manage every condition laparoscopically. Some laparoscopic surgeries may have to convert to open surgery if they turn out to be more complicated than predicted.
Advertisement
Advertisement
Before Hartmann introduced his procedure in 1921, disease in the lower bowel was treated by permanently removing the entire sigmoid colon, rectum and anus. This more severe surgery is still necessary in some cases, but it has its disadvantages. It’s more difficult for the surgeon, riskier for the patient and it’s permanent. Hartmann’s procedure offers a faster, safer and less permanent alternative for cases where the immediate condition may be critical but the long-term outlook may be more optimistic.
Advertisement
This surgery is considered relatively safe, but complications are always possible. They may include:
It may take four to six weeks to:
It may take three to six months to:
Surgery is demanding on the body, especially following a major illness such as infection or cancer. Your surgeon will consider your fitness for additional surgery between six and 12 months after the first one. If you've healed well and are in good general health, you may choose to undergo reversal surgery.
Factors that may advise against reversal surgery include:
If you’re someone undergoing Hartmann’s procedure, chances are it is saving your life. This can make the weight of the surgery easier to bear. Keep in mind that as surgeries go, Hartmann’s procedure is relatively fast and safe and the prognosis is generally good. The recovery and the adjustment to life with a colostomy are no small matter, but they're most likely saving you from cancer, systemic infection or permanent bowel dysfunction. You may even be able to reverse the procedure in six to 12 months’ time.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Some conditions like rectal and colon cancer, Crohn’s disease and ulcerative colitis may require colorectal surgery. Cleveland Clinic has the expert care you need.
