Uterine fibroids are a common type of noncancerous tumor that can grow in and on your uterus. Not all fibroids cause symptoms, but when they do, symptoms can include heavy menstrual bleeding, back pain, frequent urination and pain during sex. Small fibroids often don’t need treatment, but larger fibroids can be treated with medications or surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
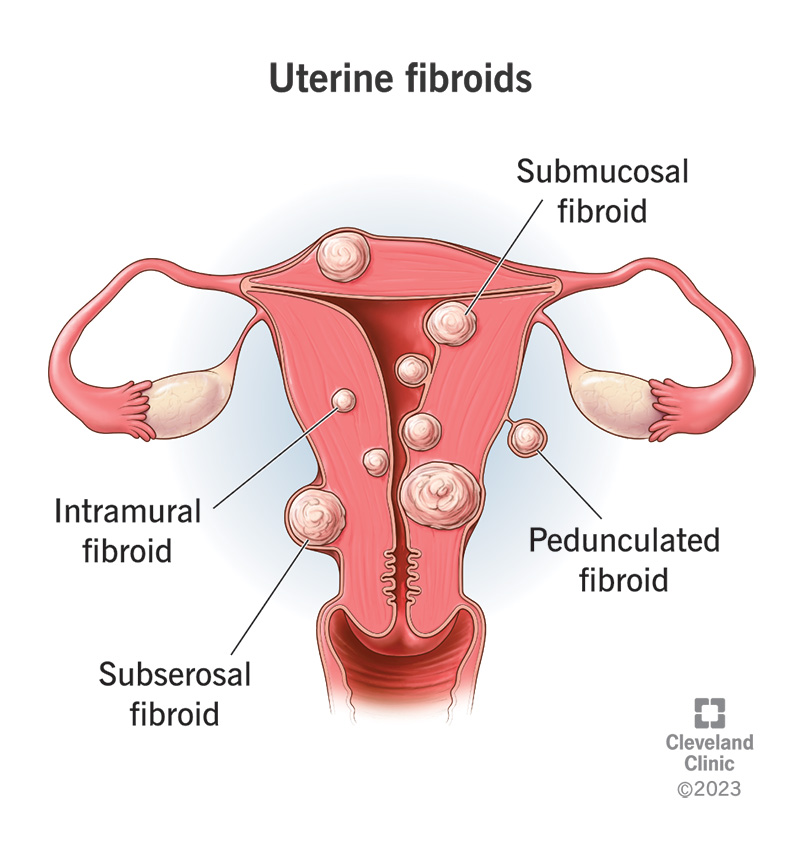
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9130-uterine-fibroids)
Uterine fibroids (also called leiomyomas) are growths made of muscle and tissue that form in or on the wall of your uterus. These growths are usually not cancerous (benign) and are the most common noncancerous tumor in females.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Uterine fibroids can cause a variety of symptoms like pain and heavy, irregular vaginal bleeding. Sometimes, a person has no symptoms and is unaware they have fibroids. Treatment for fibroids typically depends on your symptoms.
Fibroids can grow as a single nodule (one growth) or in a cluster. Clusters of fibroids can range in size from 1 millimeter to more than 20 centimeters (8 inches) in diameter or even larger. For comparison, fibroids can be as small as a seed or get as large as a watermelon. These growths can develop within the wall of your uterus, inside the main cavity of your uterus or on the outer surface of your uterus.
There are different types of uterine fibroids depending on where they’re located and how they attach. Specific types of uterine fibroids include:
Advertisement
Fibroids are a very common type of growth. Approximately 40% to 80% of people with a uterus have fibroids. They occur most often in people between 30 and 50 years old. People who haven’t had their first period (menstruation) yet typically don’t have fibroids. They’re also less common in people who’ve entered menopause.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_zew2os1y/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
What are uterine fibroids and what are the risk factors?
Most small fibroids don’t cause any symptoms and don’t require treatment other than regular observation by your healthcare provider. Larger fibroids can cause you to experience a variety of symptoms, including:
The symptoms of uterine fibroids usually stabilize or go away after you’ve gone through menopause because hormone levels decline within your body.
There are a variety of feelings you might experience if you have fibroids. If you have small fibroids, you may feel nothing at all and not even notice they’re there. For larger fibroids, however, you can experience discomfort and pain. Fibroids can cause you to feel back pain, stabbing pains in your abdomen and even pain during sex.
Fibroids are typically rounded growths that look like smooth bumps. In some cases, they can be attached with a thin stem, giving them a mushroom-like appearance.
The exact cause is unknown, but healthcare providers believe the hormones estrogen and progesterone play a role. Most fibroids happen in people of reproductive age. Studies show that fibroids tend to grow when hormone levels are higher (like during pregnancy) and shrink when hormone levels are low (like during the transition to menopause).
There are several risk factors that can play a role in your chances of developing fibroids. These can include:
Most uterine fibroids don’t cause serious complications. However, the most common complications of fibroids are:
Anemia is a condition that happens when your body doesn’t have enough healthy red blood cells to carry oxygen to your organs. Anemia can happen to people who have frequent or extremely heavy periods. Fibroids can cause your periods to be very heavy or for you to even bleed between periods. Talk to your healthcare provider if you’re experiencing symptoms of anemia while you have fibroids.
Advertisement
In many cases, a healthcare provider discovers uterine fibroids during a pelvic exam. Quite often, heavy bleeding and other related symptoms may alert your provider to consider fibroids as a part of the diagnosis. There are several tests that can be done to confirm fibroids and determine their size and location. These tests can include:
Advertisement
Treatment for uterine fibroids can vary depending on the size, number and location of the fibroids, as well as what symptoms they’re causing. If you aren’t experiencing any symptoms from your fibroids, you may not need treatment. Small fibroids can often be left alone. Some people never experience any symptoms or have any problems associated with fibroids. In these cases, your provider may recommend monitoring your fibroids with pelvic exams or ultrasounds.
If you’re experiencing symptoms from your fibroids — including anemia from excess bleeding, moderate to severe pain or urinary tract and bowel problems — you’ll need treatment to help. Your treatment plan will depend on a few factors, including:
The best treatment option for you will also depend on your plans for pregnancy in the future. Talk to your healthcare provider about your fertility goals when discussing treatment options. Treatment options for uterine fibroids can include:
Advertisement
It’s important to talk to your healthcare provider about any medication you take. Always consult your provider before starting a new medication to discuss any possible complications.
There are several factors to consider when talking about the different types of surgery for fibroid removal. Not only can the size, location and number of fibroids influence the type of surgery, but your wishes for future pregnancies can also be an important factor when developing a treatment plan. Some surgical options preserve your uterus and allow you to become pregnant in the future, while other options can either damage or remove your uterus.
Myomectomy is a procedure that allows your provider to remove the fibroids. There are several types of myomectomy. The type of procedure that may work best for you will depend on where your fibroids are located, how big they are and how many you have. The types of myomectomy procedures to remove fibroids can include:
If you aren’t planning future pregnancies, there are additional options your healthcare provider may recommend. These options can be very effective, but they typically prevent future pregnancies. These can include:
There can be risks to any treatment. Medications can have side effects and some may not be a good fit for you. Talk to your healthcare provider about all medications you may be taking for other medical conditions and your complete medical history before starting a new medication. If you experience side effects after starting a new medication, call your provider to discuss your options.
There are also risks involved in surgical treatment of fibroids. Any surgery places you at risk of infection and bleeding, and includes risks associated with anesthesia. An additional risk of fibroid removal surgery can involve future pregnancies. Some surgical options can prevent future pregnancies. Myomectomy is a procedure that only removes the fibroids, allowing for future pregnancies. However, people who’ve had a myomectomy may need to deliver future babies via C-section.
There isn’t a definitive size of a fibroid that would automatically mean it needs to be removed. Your healthcare provider will determine if surgery is necessary based on your symptoms. For example, fibroids the size of a small marble may still cause excessive bleeding depending on their location. Your healthcare provider can discuss symptoms that might require surgical intervention.
If you don’t have symptoms, treatment for fibroids may not be necessary. If you have large fibroids or your symptoms are causing you pain and discomfort, getting treatment may be the best option. Only you and your provider can decide the best course of treatment or if treatment is necessary.
Yes, you can get pregnant if you have uterine fibroids. If you already know you have fibroids when you get pregnant, your healthcare provider will work with you to develop a monitoring plan for the fibroids. During pregnancy, your body releases elevated levels of hormones. These hormones support the pregnancy. However, they can also cause your fibroids to get bigger. Large fibroids can cause the following problems during pregnancy:
Fibroids can actually shrink or grow over time. They can change size suddenly or steadily over a long period of time. This can happen for a variety of reasons, but in most cases, this change in fibroid size is linked to the amount of hormones in your body. When you have high levels of hormones in your body, fibroids can get bigger. This can happen at specific times in your life, like during pregnancy. Fibroids can also shrink when your hormone levels drop. This is common after menopause. Often, your symptoms can also get better after menopause.
Fibroids can shrink in some people after menopause. This happens because of a decrease in hormones. When the fibroids shrink, your symptoms may go away. Small fibroids may not need treatment if they aren’t causing any symptoms.
Feeling tired isn’t a common symptom of uterine fibroids. However, it’s a common symptom of anemia, which can occur when you lose too much blood. Talk to a healthcare provider if you feel excessively tired so they can determine the cause.
Yes, it’s possible that large uterine fibroids can cause your stomach to bloat or appear larger.
In general, you can’t prevent fibroids. You can reduce your risk by maintaining a healthy body weight and getting regular pelvic exams. If you have small fibroids, develop a plan with your healthcare provider to monitor them.
Contact your healthcare provider if you have symptoms of uterine fibroids, such as:
Because these symptoms are common symptoms of other gynecological conditions, discussing them with a healthcare provider is important.
It’s extremely rare for a fibroid to go through changes that transform it into a cancerous (malignant) tumor. In fact, 1 out of 350 people with fibroids will develop cancer. There’s no test that’s 100% predictive in detecting rare fibroid-related cancers. However, people who have rapid growth of uterine fibroids or fibroids that grow after menopause should be evaluated immediately.
Uterine fibroids are a common condition that many people experience during their lives. In some cases, fibroids are small and don’t cause any symptoms at all. Other times, fibroids can cause challenging symptoms like pain and heavy vaginal bleeding. Talk to your healthcare provider if you experience any kind of discomfort or pain. Fibroids are treatable.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Uterine fibroids can disrupt your life. At Cleveland Clinic, our experts help create a treatment plan that works for you and fits into your busy life.
