Hemiparesis is one-sided muscle weakness. It happens because of disruptions in your brain, spinal cord or the nerves that connect to the affected muscles. It’s a symptom you shouldn’t ignore because it can be a symptom of a stroke. If it happens suddenly, you should get immediate medical attention.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
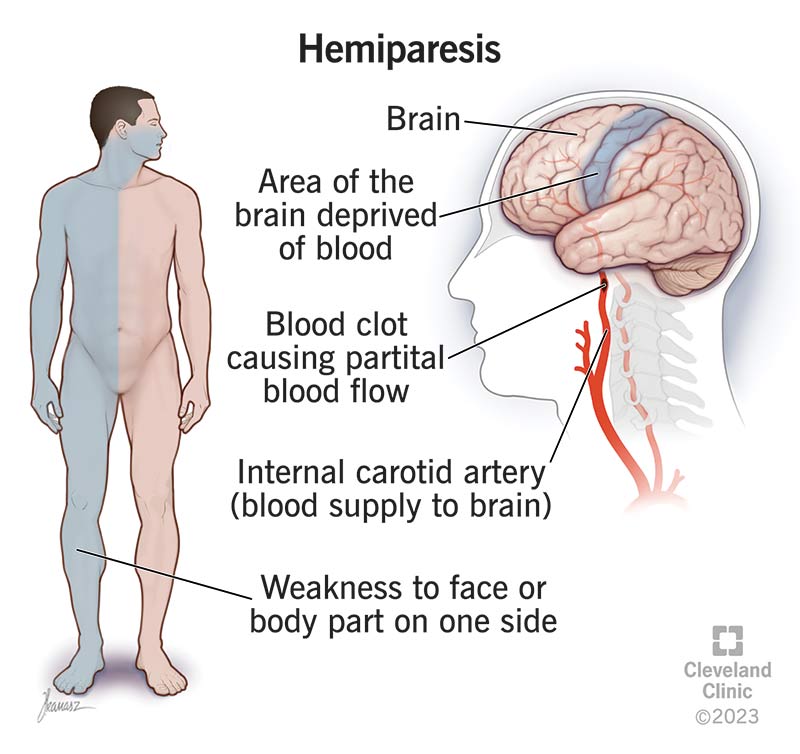
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24952-hemiparesis)
Hemiparesis is one-sided muscle weakness. It’s a key symptom of neurological (brain- or nervous system-related) problems. Some of those problems are life-threatening medical emergencies. However, hemiparesis can also happen with conditions that aren’t dangerous.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If you experience sudden hemiparesis in a limb or your face for an unknown reason, you should immediately go to the nearest emergency room (ER). Having this symptom unexpectedly can be an early sign of a stroke. You should also seek immediate medical help if you have any other signs of stroke, including balance issues, vision changes, face and arm drooping and speech difficulties.
When you have hemiparesis, the affected side of your body doesn’t have the same strength level as the opposite side. That can happen for two reasons:
The side of your body that hemiparesis affects depends on where the problem is in your central nervous system (CNS). Your brain and spinal cord make up the CNS, but the side of your body they link to depends on a quirk of your body’s structure.
Advertisement
A major part of how your CNS works depends on “decussation.” This term comes from “decussis,” the Latin word for the Roman numeral “X.” This term comes into play because there’s a point where the nerve tissue in your spinal cord “decussates.” The nerve fibers cross like an X and switch sides. Decussation happens in the brainstem, just above where your skull and spine connect.
When the problem with your CNS happens above the decussation point (in your brain), you experience hemiparesis on the opposite (contralateral) side. When hemiparesis happens because of a problem below the decussation point (somewhere in your spinal cord or peripheral nervous system), the hemiparesis symptoms happen on the same (ipsilateral) side as the problem.
The only exceptions are when the problem is in an area that relies on nerves that connect to your brain without passing through the decussation point. These points are mainly in your head and face.
Dozens of conditions and circumstances can cause hemiparesis. Some of the most common causes include:
The treatments for hemiparesis depend on the underlying cause. Some of these conditions are treatable or even curable. Others may get better on their own. Unfortunately, many of these conditions (such as spinal cord or traumatic brain injuries) can permanently damage affected parts of your nervous system. In these cases, the hemiparesis won’t go away, although it may improve to some degree.
Because there are so many different ways to treat hemiparesis, a healthcare provider is the best person to tell you more about the possible treatments in your situation. They can give you information that considers your specific condition, circumstances, health history and more.
Hemiparesis can be a sign of a stroke. Because of that, it’s not something you should diagnose or self-treat.
The only exception is if a healthcare provider previously diagnosed you with a condition that can cause hemiparesis. Migraines or seizures are examples of this.
Talk to your healthcare provider if you have a condition that can cause hemiparesis. They can tell you when this symptom is a sign that you need medical attention immediately.
Because hemiparesis is a possible stroke symptom, the risks of not treating it can be high. In the worst cases, it can result in permanent brain damage, paralysis, loss of abilities or even death.
Advertisement
Hemiparesis can happen unpredictably and for reasons that aren’t fully understood. Because of that, it’s not preventable. However, you can reduce your risk of it happening by avoiding conditions or events that can cause hemiparesis. Key ways to avoid those conditions and events include:
Advertisement
Hemiparesis should always be diagnosed and treated by a healthcare provider the first time you have it. If they diagnose you with a condition that involves hemiparesis but isn’t dangerous, they can tell you the things to watch for that mean you need medical attention.
Hemiplegia and hemiparesis are very similar symptoms, and many people — including healthcare providers — use the terms interchangeably.
Ataxic hemiparesis is when you have combined symptoms of weakness and difficulty coordinating movements. It’s generally a symptom of small-vessel blockages in your brain (lacunar stroke).
Having hemiparesis can be a scary experience, especially if it’s something you’re unfamiliar with. When it happens suddenly and unexpectedly, it’s usually a sign that you need medical attention immediately. If you experience hemiparesis or are with someone who has one-sided muscle weakness, don’t panic. Conditions that cause this symptom to appear suddenly are serious but are often very treatable if you get immediate care. With quick diagnosis and treatment, you improve the chances of having a positive outcome and returning to your usual routine and activities.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
