Chorea is a symptom that causes involuntary muscle movements. There are several possible causes of chorea. It’s a common symptom of Huntington’s disease or a neurological condition. Medications can help you manage the symptom.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Chorea is a symptom that causes involuntary, irregular or unpredictable muscle movements. It affects your arms, legs and facial muscles. Chorea comes from the Greek word that means “to dance.” It can make you look like you’re dancing, restless or fidgety.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Chorea itself isn’t life-threatening. It may occur on its own but it’s most often associated with conditions like Huntington’s disease.
The most common symptoms of chorea are movements that your body makes that you can’t control. They include:
Children diagnosed with chorea may have the following symptoms in addition to the listed involuntary movements:
Chorea symptoms may get worse if you’re:
A neurological condition affects your brain and nerves. Specific movements related to chorea can indicate an underlying neurological condition:
Advertisement
A healthcare provider, like a neurologist, will examine your symptoms and diagnose the underlying cause. If you’re unsure what type of provider to see, first speak with a primary care physician and they can make a recommendation if you need to see a neurologist or a provider who specializes in movement disorders.
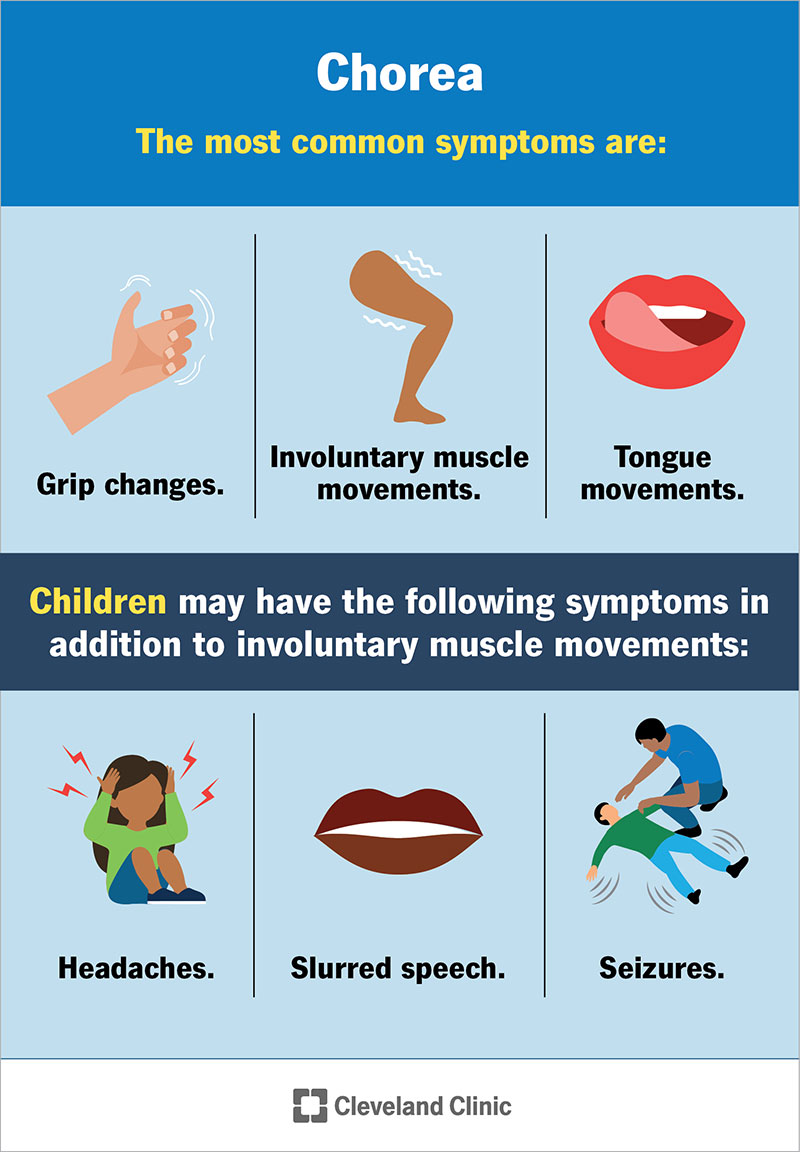
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21192-chorea)
Overactivity of a hormone called dopamine in the part of your brain that affects your movement (basal ganglia) causes chorea.
The most common causes of chorea include:
In addition, other causes of chorea include:
Chorea can happen to anyone. You may be more at risk of developing chorea if you:
Depending on the cause of chorea, complications can be severe and may include:
Advertisement
Sometimes, very mild cases of chorea that don’t interfere with your daily activities don’t need treatment. A healthcare provider will discuss your treatment options and let you know what they recommend.
The type of medication your healthcare provider prescribes to decrease your chorea symptoms varies based on the cause:
The side effects are different for each type of treatment or medication for chorea.
For example, tetrabenazine, and to a lesser extent deutetrabenazine and valbenazine, can cause suicidal thoughts and actions in people with Huntington’s disease. Before taking these medications, it’s very important to tell your healthcare provider if you have depression. People who have a history of depression shouldn’t take them without approval of their provider. If you experience suicidal thoughts, contact your healthcare provider and dial 988 (call or text) to reach the Suicide and Crisis Lifeline. Someone is available to help you 24/7.
Advertisement
Your healthcare provider will let you know about the side effects of any medication before you start taking it so you can make an informed decision about your health.
If symptoms of chorea affect your ability to eat or drink, your healthcare provider may recommend a swallow study and possible changes to your diet, like adding liquid or soft foods that are easy to chew and swallow. Your healthcare provider may suggest you meet with a nutritionist to make sure you get enough nutrients during each meal. If you’re unable to eat, contact your healthcare provider.
Some cases of chorea resolve after treatment. Other people may have to continuously manage symptoms of chorea if the underlying condition is chronic. For children diagnosed with Sydenham chorea after rheumatic fever, they usually see their symptoms resolve within two years without treatment or sooner with treatment.
You can’t prevent all causes of chorea. You can take steps to reduce your child’s risk of developing rheumatic fever by taking them to a healthcare provider to get tested for strep throat if they have a sore throat. If your child’s doctor prescribes antibiotics for strep throat, be sure your child takes them as directed and finishes all the medicine.
Advertisement
Your chorea outlook depends on the cause. Your healthcare provider will discuss your outlook with you.
For example, Huntington’s disease is progressive. This means that the condition slowly gets worse over time. It makes it very difficult to do everyday activities like getting dressed, bathing and eating. Studies estimate that people diagnosed with Huntington’s disease can live 10 to 30 years after they develop symptoms.
Children who develop Sydenham chorea after rheumatic fever usually recover within two years. Some children may have lingering behavioral or emotional complications, such as obsessive-compulsive disorder (OCD).
You should call your healthcare provider right away if you notice any unusual muscle movements. Although you may not have chorea, it’s important to get it checked out to determine what’s causing the movements.
Visit the emergency room if an involuntary movement causes you to injure yourself. It’s common for people diagnosed with chorea to fall. Your care team can help you make adjustments around your home to prevent or reduce your risk of falls and injuries.
If your child has a seizure for the first time after rheumatic fever, contact 911 or your local emergency services number.
No, not all cases of chorea are the result of Huntington’s disease, but Huntington’s disease is a common cause of chorea.
There are many causes of chorea, and the movement condition called Parkinson’s disease is one of them.
Chorea can be a frustrating symptom. Your body moves when you don’t tell it to. Even when you try to tell your body to stop, it can’t hear you. People may think you’re just clumsy. If you have irregular muscle movements that you can’t control, you should see a healthcare provider. There are several possible causes of chorea. Some are temporary and others may need lifelong management. Treatment is available to help you feel better.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Parkinson’s disease, essential tremor and dystonia are common movement disorders. And Cleveland Clinic has the expert care and support you need to manage them.
