Mastectomy is surgery to remove breast tissue. It’s a primary treatment for breast cancer. You may also have the surgery to prevent breast cancer from developing if you have a high risk of it. There are several types of mastectomies. Your surgeon will discuss your options and explain what to expect during and after surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
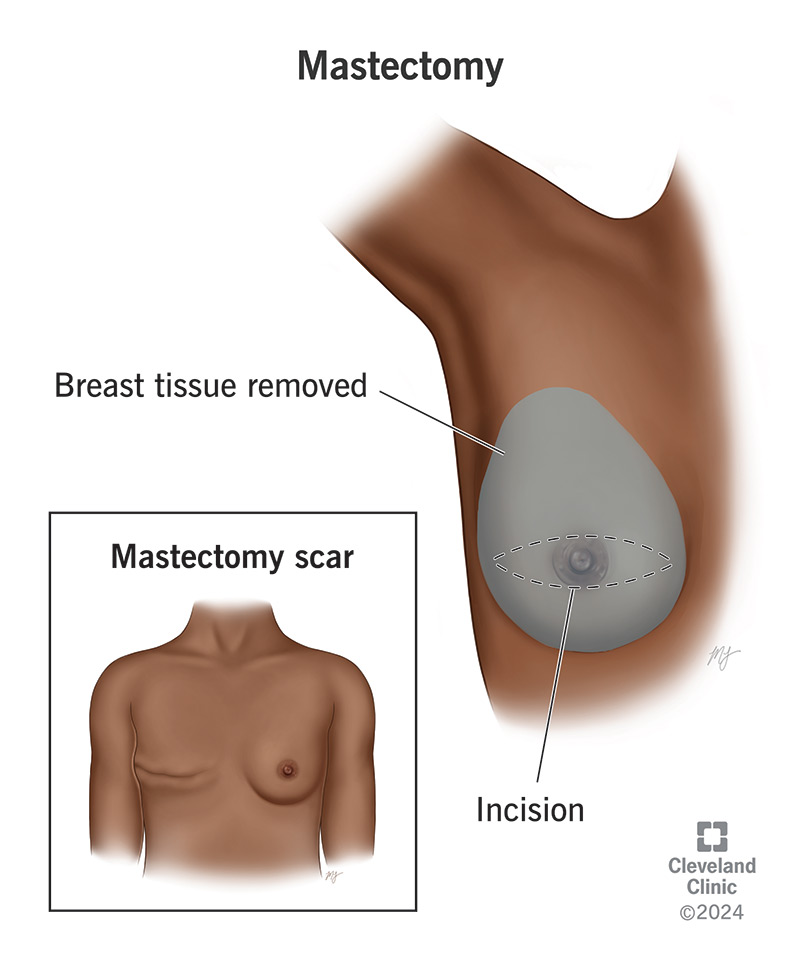
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/21221-mastectomy.jpg)
A mastectomy is a type of breast cancer surgery that removes all of your breast tissue. Healthcare providers can use it to treat most types of breast cancer. Your provider may also recommend it if you have a high risk of developing breast cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If you have breast cancer, removing the cancer cells is the best way to stop it from spreading. A mastectomy removes all the breast tissue where cancer cells are located. After a mastectomy surgery, you may possibly need other cancer treatments to kill any remaining cancer cells in the surrounding tissue.
Types of breast cancer that mastectomy treats include:
The decision to have mastectomy surgery may feel overwhelming. But you don’t have to make it alone. Your provider will help you understand your choices and what each type of mastectomy involves. Together, you can find the option that best supports your health, healing and peace of mind.
The most common types of mastectomy surgery include:
Advertisement
Other terms you may hear include:
Before surgery, you and your healthcare provider will develop a cancer treatment plan. It will include the type of mastectomy you’ll have. To restore your breast’s appearance, you may also choose to have breast reconstruction surgery after the mastectomy. Your breast surgeon usually partners with a plastic surgeon who’ll perform the reconstructive surgery.
You’ll also learn more about what to expect during your recovery. This will help you plan how to manage your daily activities after the surgery.
You may need to:
On the day of the mastectomy, you’ll get general anesthesia. That means you’ll be asleep throughout the procedure. You’ll have a tube to help you breathe and a catheter in your vein to give you fluids intravenously (IV). This keeps you hydrated during the procedure. You may also have a catheter to drain your pee.
Your surgeon will:
Advertisement
The length of the procedure depends on which type of mastectomy you have. A partial mastectomy (lumpectomy) may take an hour. A total or double mastectomy may take several hours. If you have reconstructive surgery at the same time, that will make your procedure longer.
Mastectomy complications can develop within days or weeks after surgery, and sometimes later.
Early complications from the procedure can include:
Delayed complications can include:
Advertisement
You might spend a night in the hospital, or possibly longer if you have more extensive surgery. Your healthcare team will get you up and walking on the same day as the surgery. This reduces the risk of blood clots and pneumonia from lying in bed for a long time. You’ll have pain relief as needed.
You’ll wait for lab results to figure out the next steps. Your surgeon will want to make sure they got all the cancer. They should have these results within a couple of weeks. Most of the time, there’s no need for more surgery. But sometimes, your surgeon may need to remove more lymph nodes or tissue.
You might also need other cancer treatments after surgery, like radiation therapy or chemotherapy. Some people wait to finish these treatments before starting breast reconstruction surgery. If you’ve started it, you might need additional follow-up surgeries to get the final cosmetic result you want.
Healing from a mastectomy takes time. Surgery and other treatments may cure the breast cancer, but the loss of your breast can bring many emotions. Your body will also need time to heal.
Recovery time varies depending on the type of mastectomy. But in general, you can expect the surgical wound to heal in about three weeks. Your healthcare provider will explain how to care for the wound and surgical drains at home.
Advertisement
You’ll feel tired, sore and stiff for about six weeks. Pain, swelling and bruising are common in the first weeks of recovery. Mild pain relievers can help with soreness. Your provider will teach you gentle exercises to help relieve stiffness. They may also recommend physical therapy to improve your range of motion and strength.
Many people regain some of the sensation in their chest after about two years. But your sensation may never be quite the same as before. Long-term numbness is common.
Emotional support and counseling are important after a mastectomy. There are many support groups and resources available to help you process what you’ve been through.
You may be unable to use your sore arm for up to six weeks. You won’t be able to raise your arm over your head. So, you may want to reorganize your shelves ahead of time. You also won’t be able to lift anything heavier than a gallon of milk during the first few weeks.
Follow-up appointments are important. Your healthcare team will monitor you for any complications or signs that the cancer has returned (recurred). Be sure to contact them if:
Any type of breast surgery will leave a scar and change the way your chest looks. Those changes differ from person to person. If you’re like most people, your mastectomy scars will become less noticeable over time.
What your chest looks like will depend on factors like:
Your surgeon will take steps to hide your scars as much as possible.
If tests show you have breast cancer, you might consider a mastectomy to remove it. You may also want this surgery to reduce your risk of developing breast cancer. Either way, you’re making a life-changing choice when you’re thinking about this procedure. You may feel overwhelmed by all the things you need to manage, from your emotions and planning for surgery to aftercare and recovery.
If that’s your situation, remember that your healthcare team is ready to help. They understand your concerns and can answer your questions. They’ll also recommend resources like breast cancer support groups, which can connect you with people who’ve experienced what you’re going through.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Having a lumpectomy or mastectomy is the first step toward healing from breast cancer. Cleveland Clinic breast cancer surgeons offer expertise and compassion.
