Birth control is any medicine, device or method people use to prevent pregnancy. Types of birth control can include pills, intrauterine devices (IUD), vasectomy and condoms. Some forms of birth control work better than others.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
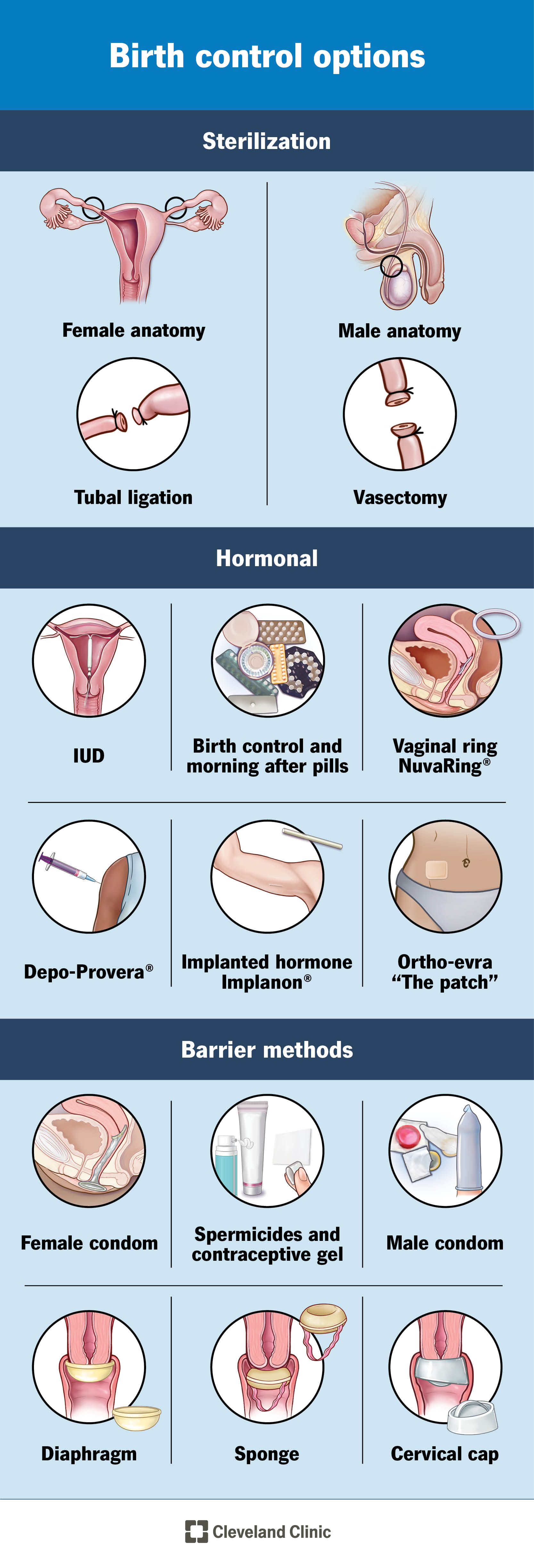
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/11427-birth-control-options.jpg)
Birth control (also called contraception) is how you prevent pregnancy. There are many different types of birth control. Birth control only works when you use it correctly. Take the time to understand how each type of birth control works and how you use it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If you're sexually active and don't want a baby, use birth control. A pregnancy can happen any time you have unprotected sex.
By learning more about birth control options, you can decide which method is best for you and your partner. Consider the following factors when making your decision:
Each form of birth control works slightly different. Some of the ways it works include:
The most effective form of birth control is to not have sexual intercourse (abstinence). Even for the most motivated couples, this can be difficult to maintain. So, it’s important to have a backup form of birth control in mind.
Advertisement
Birth control only works when you use it correctly and consistently. Forms of birth control that are more convenient and don’t require much maintenance are usually most effective. These forms include the birth control implant, intrauterine devices (IUDs) and sterilization.
Methods of birth control like fertility awareness or pulling out are least effective at preventing pregnancy.
Doubling-up on birth control is typically best — like using a condom and a birth control pill. That’s because you’re protecting against STIs, using a barrier method, and taking hormonal medication all at the same time.
Before you choose a method, you should discuss birth control with your partner and your healthcare provider. Birth control methods are only effective if you use them properly. Make sure that you understand how to use the method you choose.
Birth control methods include:
A condom is a thin covering made of latex, plastic or lambskin that is rolled over an erect penis. The covering prevents semen, the fluid that contains sperm, from entering your vagina. Condoms may tear or rip easily, making them less effective than other birth control methods.
A condom is rolled over an erect penis before sexual intercourse. Use a new condom every time you have sex.
You can purchase condoms at most drug or grocery stores.
Condoms are about 85% effective if they’re worn before intercourse begins and don’t rip.
Even though they don’t provide 100% protection, condoms are one of the best options for protection against STIs. Use only water-based lubricants, such as K-Y Jelly® or Astroglide® with condoms. Oil-based lubricants (Vaseline® or baby oil) can cause condoms to break. If a condom breaks, you should consider emergency contraception.
Spermicide is a gel, cream or suppository that prevents sperm from reaching an egg. It contains chemicals that damage sperm, so they can’t swim up to an egg. You must use spermicide exactly as directed for it to be effective. There’s also a prescription-only vaginal gel that works like a spermicide. It works by lowering the pH in your vagina, which makes it hard for sperm to swim.
Advertisement
You place spermicide and vaginal gels inside your vagina at least 15 to 30 minutes before sexual intercourse. Most spermicides work for about an hour before you need to reapply it. Reapply spermicide every time you have sex and don’t wash it out after sex.
Spermicides are available at most drug or grocery stores. The vaginal gel that reduces pH (Phexxi®) is available with a prescription.
If you use spermicide by itself, it’s only 70% effective in preventing pregnancy. If you use spermicide with another barrier method of birth control, it can be 94% effective. A vaginal gel (prescription only) is about 85% to 93% effective.
Spermicide offers no protection against STIs. In fact, it may actually increase your risk. That’s because the chemicals in spermicide irritate your vagina and make it easier for infection to enter your body.
A vaginal diaphragm is a flexible, reusable dome-shaped cup that you place inside your vagina to prevent pregnancy. It stops sperm from getting into your uterus by blocking your cervix. You must use a water-based spermicide or contraceptive gel with a diaphragm.
A diaphragm looks like a small hat or cup. You bend it in half and slide it up into your vagina so it covers your cervix. Insert your diaphragm approximately one to two hours before sex. Remove it six to 24 hours after having sex. Add spermicide around the rim of the diaphragm before intercourse for maximum protection.
Advertisement
Some diaphragms come in different sizes. It requires a visit to a healthcare provider for a pelvic exam so they can fit you for a diaphragm. Getting a properly-fitting diaphragm is important. If you lose or gain more than 10 to 15 pounds, a provider may need to refit your diaphragm. Other diaphragms, however, like the Caya® is a “one-size-fits-most” diaphragm and doesn’t require a fitting.
Vaginal diaphragms are about 87% effective, but it can be as high as 94% effective when you use it correctly (with spermicide) and consistently.
Using a diaphragm and spermicide doesn’t protect against some STIs, including HIV (the virus that causes AIDS).
A cervical cap is a thimble-shaped cup made out of silicone or soft rubber that fits snugly over your cervix.
First, coat the cap in spermicide. Then, insert the cap into your vagina and up against your cervix. The cap blocks your cervix, and the spermicide paralyzes the sperm. You can insert the cervical cap up to six hours before sexual intercourse. Don’t remove your cervical cap for at least eight hours after sex. The cap can be kept in place for up to 48 hours. Make sure to use spermicide exactly as directed.
You must visit your healthcare provider and get a pelvic exam so that you can be fitted for a cervical cap. Like a diaphragm, it’s only effective when it fits properly.
Advertisement
A cervical cap is about 78% effective at preventing pregnancy, but it can be 85% effective if you use it with a spermicide.
Using a cervical cap and spermicide doesn’t offer as much protection against STIs as condoms.
A female condom is a lubricated plastic tube that has a flexible ring at each end. One end of the tube is closed.
Before sexual activity begins, insert the condom into your vagina so that the closed end of the tube covers your cervix, and the other end slightly covers your labia (the lips on the outside of your vagina). The condom blocks sperm from entering your uterus. You remove the condom immediately after sex.
A female condom is available at drug and grocery stores without a prescription.
About 21% of people get pregnant each year despite using a female condom.
Female condoms provide some protection against STIs, but a male condom provides the best protection.
A vaginal sponge is a small, donut-shaped device that contains spermicide. It acts as a barrier between sperm and your cervix.
You wet the sponge with water, then place it into your vagina so it covers your cervix. Once it’s moist, it releases spermicide. The sponge contains enough spermicide to last about 24 hours. This means you can put it in up to 24 hours before you have sex. Always leave it in place for six hours after sex. You shouldn't leave a sponge inside your vagina for more than 30 hours.
The sponge is available without a prescription at most drug and grocery stores.
A birth control sponge is between 76% and 91% effective at preventing pregnancy (depending on if you use it correctly). The sponge is also more effective if you've never given birth.
The sponge is associated with higher rates of vaginal infections and doesn’t protect against STIs.
Nexplanon® is a small rod (the size of a matchstick) that your provider places under the skin of your upper arm. It delivers a steady stream of the hormone progestin and lasts about three years before it needs removed or replaced. Some people like the convenience of an implant because it requires little to no maintenance, doesn’t interfere with the spontaneity of having sex and can be kept secret.
A healthcare provider inserts the implant in their office. First, they numb an area in the inside of your upper arm so you don’t feel pain. Then, they use an applicator to place the implant just underneath your skin. They cover the area with a bandage. A healthcare provider must remove your birth control implant (you can’t do it yourself).
A healthcare provider must prescribe a birth control implant.
Birth control implants are almost 100% effective. It’s the most effective form of reversible contraception available.
Contraceptive implants come with risks and may not be right for you. The most common side effect of an implant is irregular bleeding, though the bleeding tends to be light. This typically improves after six to 12 months, but some people completely stop getting their periods. Other side effects include sore breasts and headaches.
An intrauterine device (IUD) is a small, flexible, T-shaped device you put in your uterus to prevent pregnancy. There are two types of IUDs:
The copper ParaGard T380A®, can be kept in place for 10 years. The copper stops sperm from making it through your vagina and uterus to reach an egg.
The progestin IUDs include:
These IUDs work by causing your cervical mucus to become thicker so sperm can’t reach an egg. The hormone also thins the lining of your uterus, so menstrual bleeding becomes lighter.
IUDs are one of the “get it and forget it” forms of birth control. This means once you get it, you can forget it because there is no daily or monthly maintenance.
After a pelvic exam, a healthcare provider places the IUD into your uterus. It’s only available with a prescription.
The IUD is close to 100% effective.
No, an IUD shouldn’t hurt. You may feel uncomfortable or have light cramping after your provider puts it in. The same goes for getting your IUD out — there may be brief discomfort.
Side effects are different depending on the type of IUD you have. Copper IUDs may cause more painful and heavy periods. Some people prefer copper IUDs because it doesn’t contain hormones. The most common side effect of progestin IUDs is irregular bleeding. This typically improves after six to 12 months. Some people may also stop getting their periods completely. A provider must remove your IUD. In the very rare chance pregnancy occurs while having an IUD, there is a greater chance that the pregnancy is an ectopic pregnancy.
IUDs can also be used for emergency contraception within 120 hours (five days) of having unprotected sex. It’s actually more effective as an emergency contraception than the morning after pill.
Includes estrogen containing birth control pills, the contraceptive vaginal ring (NuvaRing®) and patch (Xulane®).
The pill, patch and ring are medications that you take to prevent pregnancy. You take the pill daily, insert the vaginal ring once a month and change the patch weekly. Most hormonal contraception contains two different hormones (estrogen and progestin). All of these forms of birth control work by preventing ovulation.
You take a pill at the same time every day. There are several different types of pills. Some are designed to allow for a monthly period, while others allow for a longer time between periods or no period at all. You replace a vaginal ring every month to allow for your period. A birth control patch releases hormones through your skin. You replace your patch once per week. All of these methods require regular, consistent use. If you forget to use it, irregular menstrual cycles are common and you can get pregnant.
Hormonal birth control is available by prescription only.
Combined hormonal contraceptives have the potential to be 99% effective if you use it correctly. However, most people don’t use it correctly, so the effectiveness is around 91%. While not as effective as an IUD or implant, hormonal contraception like the pill is much more effective than barrier methods like condoms.
The pill can cause minor side effects in the first several months of use, including:
Contraception that contains estrogen increases your risk of blood clots. Talk to a healthcare provider to make sure estrogen-containing contraception is right for you. There are benefits to hormonal contraception like lighter, more regular periods and less menstrual cramping. Birth control pill users may also notice an improvement in acne and PMS.
These are birth control pills that contain only one hormone (progestin).
Minipills work by thickening your cervical mucus so sperm can’t reach an egg. The hormone in the pills also thins the lining of your uterus, so menstrual bleeding is lighter. For the minipill to be most effective, it’s very important you take a mini pill at the same time each day. Progestin-only “minipills” are available with a prescription.
Like combination birth control pills, progestin-only pills can be 99% effective. In reality, they’re about 91% effective because most people don’t use them correctly.
The most common side effect of a progestin-only pill is irregular bleeding, though the bleeding tends to be light. This typically improves after six to 12 months. The minipill is a good alternative for people who are breastfeeding or who can’t take estrogen.
Depo-Provera® is a form of the hormone progestin. It stops you from ovulating and thickens your cervical mucus to prevent sperm from reaching an egg.
The birth control shot is an injection. Your provider injects it into your upper thigh or arm. Each injection provides protection against pregnancy for about 12 weeks (or three months). Some providers allow you to inject yourself at home with a low-dose version (Depo-Subq Provera 104®).
Depo-Provera® must be prescribed by a healthcare provider. They’ll inject you with the hormone in their office. You may be able to inject yourself at home if you use the lower dose version of the shot.
The Depo-Provera® shot has the potential to be 99% effective. However, 6% of people get pregnant each year on the shot because they don’t get the injections on time.
Depo-Provera® may cause irregular bleeding. People who use it for more than one year stop getting their period while on the medication. This is the only contraceptive that may cause weight gain. It may be slightly harder to predict when your fertility will return once you stop Depo-Provera® (compared to other birth control methods).
The rhythm method (or calendar method) teaches you to recognize when you’ll ovulate. This allows you to determine your fertile days, or the days you’re most likely to get pregnant. You avoid having sex on the days you’re fertile.
You use a calendar to chart and predict ovulation. It involves tracking and recording your cycle for several months until you’re able to predict your menstrual cycle.
It’s one of the least effective forms of birth control. Even when it’s done correctly, it’s only effective about 75% to 88% of the time.
The rhythm method doesn’t work if you have irregular menstrual cycles. The benefits are that it has no side effects and is inexpensive.
The cervical mucus method of birth control involves analyzing your vaginal discharge to identify when you’re most fertile. You avoid sexual intercourse during your fertile time.
You can check your cervical mucus using your finger or by looking in your underwear. Fertile cervical mucus is slippery, clear and has the texture of egg whites. Thick, pasty discharge means you aren’t fertile. Learning the stages your cervical mucus goes through each menstrual cycle helps you predict ovulation.
The cervical mucus method can be up to 88% effective. In most cases, it’s about 75% effective.
Tracking your cervical mucus is time consuming and requires dedication. It involves avoiding intercourse on the days you’re fertile, which may be up to two weeks. It can sometimes be hard to pinpoint which days are safe for intercourse.
Taking your basal body temperature is a way to identify ovulation. You must have a thermometer that measures temperatures to at least one-tenth of a degree for it to work.
Record your temperature every morning before getting out of bed (before you even stand up). Basal body temperature typically rises less than one-half of a degree after you ovulate. Once your temperature increases, you’re safe to have unprotected sex for up to three days. It may take a few cycles to determine when this rise occurs each month.
It’s not effective when used alone because it only tells you that ovulation has occurred, not that it’s about to. Since you can get pregnant up to five days before ovulation, it’s very unreliable.
Recording your temperature at rest each morning takes a lot of dedication. While inexpensive to use, it doesn’t offer as much protection against pregnancy as barrier methods or hormonal birth control.
Abstinence is the only birth control that is 100% effective. It means you never have sexual intercourse. It’s also the only way to protect yourself from STDs.
Don't let someone pressure you into having sex if you don't feel ready. It’s an important decision with serious emotional and physical consequences.
Emergency contraception is a form of birth control that you can use within 120 hours (five days) of having unprotected sex. It’s most effective in preventing pregnancy if you use it within three days of unprotected intercourse.
The most effective morning after pill contains ulipristal (brand name: ella®). It’s only available by prescription. Several over-the-counter options are available and all contain levonorgestrel (many generic names including Plan B One-Step®, Take Action®, etc.).
The pills prevent pregnancy by temporarily blocking eggs from being produced (delaying ovulation).
You can purchase levonorgestrel pills over-the-counter (without a prescription) at your local drug store. Ulipristal (ella®) is available by prescription only.
Emergency contraceptive pills can be up to 90% effective when taken within 72 hours of unprotected intercourse. However, no pills will work if you have already ovulated. This is why it’s important to take it as soon as possible after intercourse.
Yes, both copper-containing IUDs (Paragard®) and progestin-containing IUDs (Mirena® or Liletta®) can be used as a form of emergency contraception when used within 120 hours (five days) of having unprotected sex. This is the most effective form of emergency contraception. The benefit of using IUDs for emergency contraception is that you’re seeking a method of birth control and you’re preventing future unwanted pregnancies.
Progestin-containing IUDs work by causing your cervical mucus to become thicker so sperm can’t reach an egg. The hormone also thins the lining of your uterus, so menstrual bleeding becomes lighter. The copper-containing IUD works by stopping the sperm from reaching the egg.
A healthcare provider prescribes and inserts IUDs.
IUDs can be close to 100% effective at preventing pregnancy when inserted within five days of having unprotected sex.
Menstrual irregularities are common after you take emergency contraception. However, if you don’t get your period within a few weeks of taking emergency contraception, you should take a pregnancy test. It's important to use condoms or abstain from intercourse for the next five days after taking emergency contraception, otherwise you can get pregnant. If you find yourself taking emergency contraceptive pills frequently, speak to a healthcare provider about more effective ways to prevent pregnancy. The benefit of using IUDs as a form of emergency contraception is that you are taking proactive steps to protect yourself from future unwanted pregnancies.
Salpingectomy is a surgical procedure to permanently remove your fallopian tubes. This prevents an egg from reaching your uterus. It also blocks sperm from your fallopian tube, where fertilization typically occurs. Provider often perform this surgery over tubal ligation (where the fallopian tubes are tied off but not completely removed), because in the very rare chance you do get pregnant with a tubal ligation, there's a higher chance of having an ectopic pregnancy.
Your healthcare provider performs salpingectomy while you’re asleep. They make two to three small incisions (cuts) in your abdomen, then insert a tool called a laparoscope. They are able to seal and completely remove your fallopian tubes through the laparoscope.
This procedure is almost 100% effective.
Female sterilization is permanent. You should not get permanent sterilization if you feel you may change your mind about wanting to get pregnant in the future. While in very rare cases it can be reversed, this operation is not without risk, and can be very expensive. It doesn’t protect against STDs.
A tubal ligation is a procedure to block your fallopian tubes. A surgeon clamps, ties or blocks your fallopian tubes to prevent pregnancy. The procedure is similar to a salpingectomy, but your fallopian tubes aren’t completely removed. In the rare chance you’d get pregnant after a tubal ligation, you’re at higher risk for an ectopic pregnancy.
Tubal ligation is about 100% effective.
A vasectomy is a procedure to seal the vas deferens, the tubes in the male reproductive system that carry sperm. Without sperm, pregnancy can’t occur.
Healthcare providers typically perform a vasectomy in an office or surgical center under a local anesthesia (numbing the area). Your surgeon makes a small incision in your scrotum to access the vas deferens tubes. Then, they tie off or cut the tubes.
Vasectomies are almost 100% effective, but failure is possible. It is important to know that it does not provide immediate protection against pregnancy. You will need to use an additional form of birth control for a few months after the procedure, until your provider confirms there are no sperm left in your semen.
Sterilization doesn’t protect against STDs. In some cases, your provider can reverse a vasectomy. There are fewer risks of complications with a vasectomy than a laparoscopic salpingectomy.
The pull out method (or withdrawal method) is when a person’s penis “pulls out” of a person’s vagina before ejaculation (or cumming). Removing your penis before sperm comes out is one way to prevent pregnancy, but it’s very ineffective. That’s because it’s hard to do. Even a tiny amount of semen (cum) can get a person pregnant. About 1 in 5 (or 20%) of people will get pregnant each year if pulling out is their only method of birth control.
Condoms are the best way to prevent STIs. However, condoms aren’t the most effective at preventing pregnancy. Condoms work best when they’re used with another type of birth control.
By learning more about the different forms of birth control, you can decide what method is best for you. Some things you should consider include how often you have sex, your overall health and your future plans for children. Another important factor is convenience. Certain birth control options require daily upkeep (like a pill) to be effective, while other methods (like an IUD) are “get it and forget it” because they last for years. Some birth control methods are easier to keep hidden from others, and some are better at preserving sexual spontaneity than others. Discuss your options for birth control with a healthcare provider. They can help you understand how each form of contraception works as well as the risks and benefits of each.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Your birth control needs to work for you. At Cleveland Clinic, we help you find the right birth control option to fit your goals and lifestyle.
