Wet macular degeneration is when new blood vessels grow underneath the macula, a critical part of your retinas. These vessels can leak, causing damage and scarring to an area essential for the center of your visual field. It’s treatable, but preventing or delaying it is best. Once it starts, early detection, diagnosis and care are vital.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
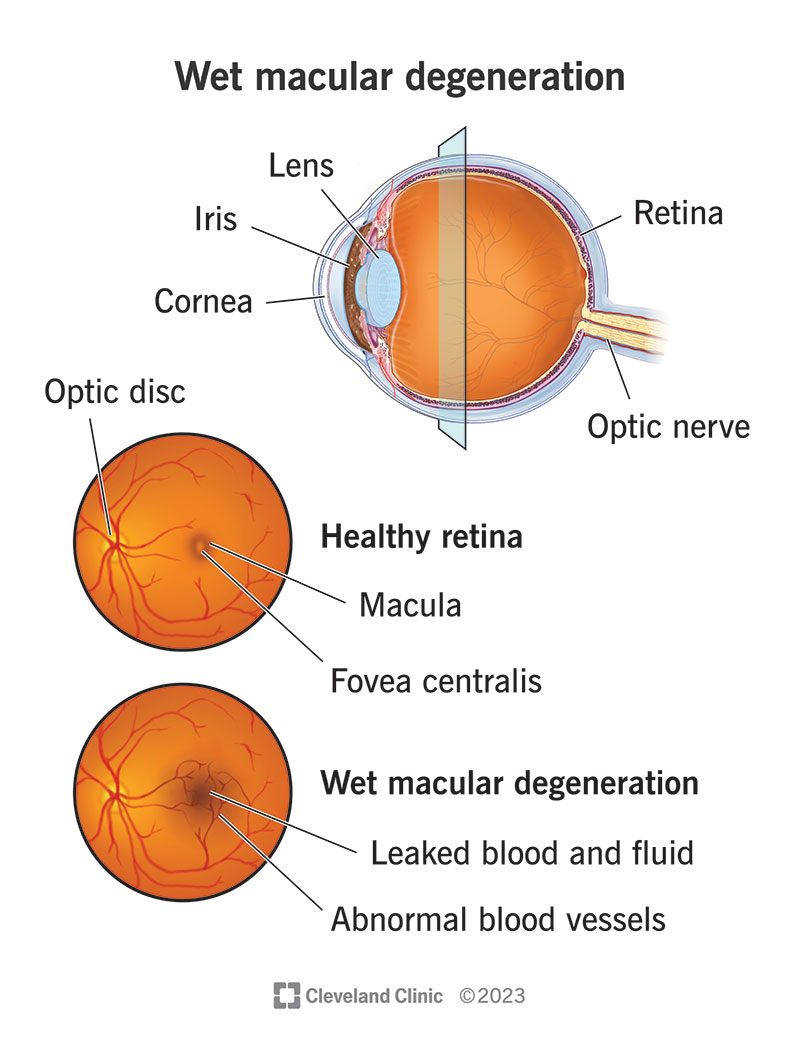
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/wet-macular-degeneration)
Wet age-related macular degeneration (WMD) is the advanced form of age-related macular degeneration (ARMD), a condition that can cause permanent central vision loss. WMD is an advanced form of age-related macular degeneration. It happens when age-related changes in your eyes worsen and cause new blood vessels to grow and leak underneath the retina.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When you have WMD, new vessels grow and disrupt existing retinal tissue, causing damage and vision loss. The leaked blood can also cause scar tissue to form, further distorting and damaging the macula.
Over time, the leaked blood and scar tissue can cause permanent vision loss. However, early detection and treatment can prevent that kind of permanent damage or stop it from further damaging your vision. If you notice vision changes that could be WMD, you need to see an ophthalmologist as soon as possible.
The formal name for this condition is exudative (pronounced either “EX-yoo-dat-iv” or “EGS-yoo-dat-iv”) macular degeneration or neovascular macular degeneration. “Exudate” is a medical term for leaked fluid, which is where this condition’s formal name comes from.
Your odds of developing ARMD increase with age, and it’s the leading cause of vision loss for adults over 60. About 10% to 20% of ARMD cases are the wet form, meaning between 10 million and 20 million adults worldwide have WMD. Between 1 and 2 million of those cases are in the U.S.
Wet macular degeneration causes painless central vision loss. It can affect both eyes, though it may do so unevenly.
Symptoms can include:
Advertisement
WMD isn’t a condition with a single cause. Instead, it’s a condition where many risk factors or contributors can add up and make this condition more likely to develop.
The risk factors and contributors that can play a role in developing WMD include:
The main complication of wet macular degeneration is central vision loss. Without treatment, about 80% to 90% of people with WMD will eventually have vision loss severe enough that they meet the criteria for legal blindness.
An eye care specialist, such as an ophthalmologist or a retina specialist, can diagnose WMD with a combination of methods.
The first step is a routine eye exam. During that exam, they can view your retinas directly. That’s possible either with a handheld instrument called an ophthalmoscope, or by dilating your pupils and doing a slit lamp exam. They may also use an Amsler grid eye test, a simple grid chart that makes it easier to see distortions in your vision (the distortions in your retina will distort the way the grid looks to you).
In addition to an eye exam and the slit lamp exam, an eye care specialist can also use noninvasive diagnostic imaging tests. These let your eye specialist look at the internal structures and blood vessels at the back of your eye. The possible tests include:
Wet macular degeneration is very treatable if detected early enough. There are two main ways to treat WMD: medications and laser procedures.
Advertisement
Medication treatments involve blocking vascular endothelial growth factor (VEGF), a protein your body uses for growing new blood vessels. Blocking VEGF stops the formation of new blood vessels. The medications that can do this are given via an injection into your eye.
These medications include:
The goal of laser procedures for WMD is to stop new blood vessels from growing and shrink them, if possible. Whether laser surgery is an option depends on where the new blood vessels are growing under your macula and other factors. Injections are more common than laser procedures.
Your eye care specialist is the best source of information about your treatment options. The information they give will be most relevant and helpful for your specific case. They can also tell you about the possible side effects or complications and which treatment will most likely help you.
The outlook for WMD depends on several factors. They include:
Because so many factors can play a role, your outlook can vary widely. Your eye care specialist can tell you more about the likely outlook in your specific case.
Advertisement
There are so many contributing and risk factors for WMD that it’s impossible to prevent it entirely. But there are things you can do to reduce your risk of developing it or delay when it happens.
Some of the most important ways to prevent or delay WMD start when you have dry macular degeneration, the less-advanced form of ARMD. Steps your eye specialist could recommend include:
Advertisement
There may be other steps you can take to help yourself avoid vision loss from WMD. If you have any questions or concerns about steps you can take, ask your eye specialist. They can offer guidance and resources that can help you.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_a9ze5zwc/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn tips to manage wet age-related macular degeneration.
WMD can be very disruptive once it starts to cause vision loss. It can impact your ability to live independently and go about your usual routine and activities.
If you already have vision loss from WMD, there are still things you can do to help yourself. They include:
Your eye specialist will recommend a follow-up visit schedule to manage your WMD and adjust your treatments if necessary. These visits are a crucial part of limiting vision loss.
You should also call your eye specialist immediately if you notice changes in your vision, such as distortions you can see while testing your eyes with an Amsler grid.
Some questions you may want to ask your eye specialist include:
Vision is a sense that most people use nearly constantly throughout their daily lives, often without thinking about it. Vision loss can be disruptive and upsetting. But there are things you can do to limit the damage, prevent further vision loss and adapt to any existing changes.
Talking to your eye care specialist is the best way to learn what you can do about this condition. They can guide you on steps and changes that can help you. They’re there to help you so you don’t have to face this condition or its effects alone.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you see dark or blank spots when reading or looking at people, Cleveland Clinic can help. We offer personalized macular degeneration diagnosis and treatment.
