Ocular rosacea causes painful inflammation in your eyes and the skin around them. There’s no cure that will make it go away permanently. But you should experience fewer flare-ups and milder symptoms once you learn to avoid your triggers. Your provider and eye care specialist will also help you find treatments that manage your symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
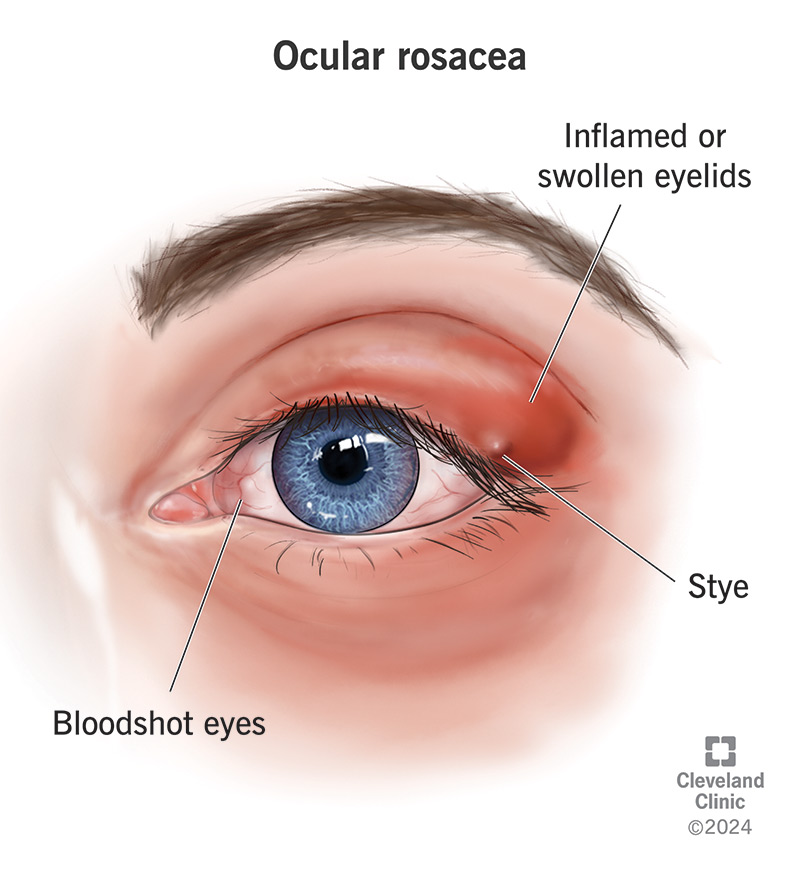
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/ocular-rosacea)
Ocular rosacea is a condition that causes inflammation in your eyes and the skin around them. It’s a specific type of rosacea — a skin disease that causes inflammation and discoloration on your whole face. Healthcare providers sometimes call ocular rosacea “meibomian gland dysfunction.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Ocular rosacea might make your eyes and the skin around them feel irritated, painful, itchy and uncomfortable when you’re having a symptom flare-up.
There’s no cure for ocular rosacea, but a healthcare provider or eye care specialist will help you manage your symptoms and avoid the triggers that make them worse.
Ocular rosacea symptoms usually come and go in episodes called flares or flare-ups. Which symptoms you have may change over time or between flare-ups.
The most common ocular rosacea symptoms are changes you can feel and see on the skin around your eyes, including:
Ocular rosacea can cause symptoms in your eyes, too. You might experience:
Many people picture rosacea causing “redness” on only white or fair skin. But people with darker skin can have ocular rosacea, too. Many of the symptoms are the same, but rosacea’s trademark discoloration might be harder to notice. You might not be able to see it at all. If you can see discoloration around your eyes, the affected skin might be darker than your usual skin tone.
Advertisement
Experts aren’t sure what causes ocular rosacea. Some possible explanations include:
Even though researchers aren’t certain what causes ocular rosacea, they’ve found some triggers that lead to flare-ups. A trigger is something that causes symptoms to flare up or get worse.
Common ocular rosacea triggers include:
It’s rare, but untreated ocular rosacea can damage your eyes and permanently affect your vision.
You also have an increased risk of eye infections if symptoms like itching or burning make you reflexively touch your eyes. Try to avoid rubbing your eyes, and make sure you wash your hands before touching your eyes and face.
A healthcare provider or eye care specialist will diagnose ocular rosacea with a physical exam and eye exam. They’ll examine your skin and eyes. They might check your vision, too. Tell your provider about all the symptoms you’ve felt, even if they got better before your appointment.
Your symptoms, medical history and any triggers you’ve noticed are the only way to diagnose ocular rosacea, so every detail you share can help your provider diagnose it correctly.
The most important part of managing ocular rosacea is knowing — and avoiding — your triggers. It might not always be possible, but avoiding activities, foods or situations that might trigger ocular rosacea flare-ups is the best way to minimize how often you experience symptoms.
There’s no cure, but your provider or eye care specialist will suggest treatments that help you manage symptoms, including:
You should avoid foods and drinks that trigger your ocular rosacea symptoms. For most people, this includes spicy foods and alcohol. Your triggers will be unique to you.
You should feel better a few weeks after starting new treatments. If you need prescription eye drops or other medications, it might take anywhere from a few days to a few weeks for them to start working.
Advertisement
The treatments won’t cure ocular rosacea, but they should relieve your symptoms and make you more comfortable during a flare-up.
You’ll probably need to manage ocular rosacea symptoms for a long time (maybe for the rest of your life). There’s no cure for it, so there isn’t any treatment that can make it go away permanently.
Most people with ocular rosacea experience fewer (and less severe) flare-ups once they learn to identify and avoid their triggers and find treatments that help manage their symptoms.
Some of the best ways to prevent ocular rosacea flares include:
It might help to keep a list or a journal of what triggers your symptoms. This can be especially useful right after your diagnosis.
Make sure you’re following the treatment plan you work on with your provider. Even when you’re not having a flare-up, it’s important to use your medicines and other preventive treatments as often as your provider prescribes.
Visit your healthcare provider or eye care specialist if it feels like your symptoms are getting worse or if you’re experiencing flare-ups more often.
Advertisement
Make sure to mention any new or different symptoms as well. Your provider can adjust your treatment options to fit your current symptoms as they change over the course of your life.
Go to the ER if your symptoms include:
Some researchers think ocular rosacea might be an autoimmune disease, but we don’t have enough proof to say for sure that it is.
Autoimmune diseases happen when your body’s immune system attacks your body instead of protecting it.
Some studies have found that some people with ocular rosacea experience flare-ups after triggers make their immune system become overly active, but this isn’t true for all people.
Being diagnosed with any chronic condition means you unexpectedly have a lifelong issue to manage. That includes ocular rosacea. It can seem overwhelming at first, but as you learn what helps you manage your symptoms and which triggers to avoid, you should be able to get into a good rhythm of feeling like yourself again. Your healthcare provider or eye care specialist will help you come up with treatment plans and strategies to avoid your triggers.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic’s ophthalmologists and optometrists have the highest training available. We provide exams, vision correction and care for many eye conditions.
