A popliteal aneurysm is an enlarged section of an artery behind your knee. The aneurysm may be on only one side or all around your artery. You may also have one behind your other knee. Many people don’t have symptoms unless their popliteal aneurysms break open or they have blood clots. Open or minimally invasive surgery treats this condition.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
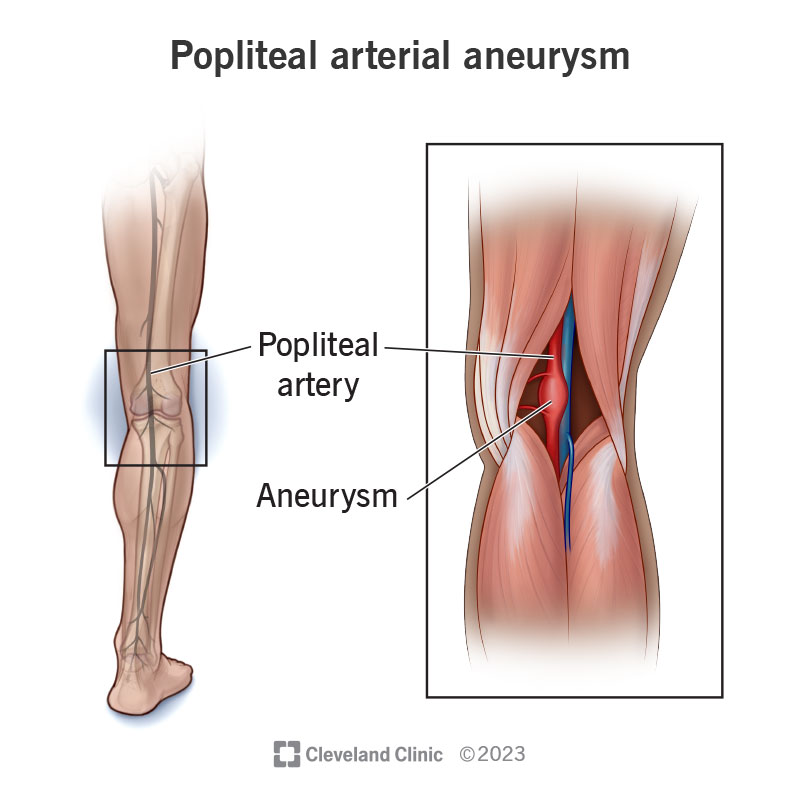
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/popliteal-arterial-aneurysm)
A popliteal aneurysm is a ballooned-out part of your popliteal artery, which is behind your knee. Half of the people with popliteal aneurysms will have them in both legs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Popliteal aneurysms can cause issues if they burst (rupture), send a clot down your leg (embolize) or block artery flow (thrombose). Some people can lose their legs or even their lives when this condition takes a turn for the worse.
Popliteal aneurysms happen in 1 in 100,000 women and 7 in 100,000 men.
Popliteal aneurysms aren’t common, but they’re second only to abdominal aortic aneurysms (the most common kind of aneurysm). These two are related, and nearly half of people with a popliteal aneurysm will also have an abdominal aortic aneurysm. So if a provider finds either aneurysm, it’s important to look for the other.
Usually, people don’t have any popliteal aneurysm symptoms. However, when symptoms do occur, the aneurysm can be life-threatening. An aneurysm that bursts can cause pain behind your knee, swelling and bruises. When the aneurysm has a clot and some of it escapes down your leg or the aneurysm blocks off completely (thromboses), it can cause a lack of blood flow to your leg. Symptoms of this can be:
Researchers aren’t sure what causes a popliteal aneurysm. Possible popliteal aneurysm causes include:
Advertisement
Popliteal aneurysm risk factors include:
Complications of a knee aneurysm include:
Diagnosing a popliteal aneurysm can be difficult. A deep vein thrombosis (DVT) or a Baker’s cyst can appear similarly, so ruling these conditions out is helpful.
To make a popliteal aneurysm diagnosis, a provider will examine the back of your knee. They may be able to see and feel the enlarged artery there and it may throb with your pulse.
A provider may describe your popliteal aneurysm as fusiform (ballooning out all around) or saccular (only one side of your artery balloons out).
Imaging tests can help a provider make a diagnosis and take measurements for planning a repair.
These tests include:
If your provider diagnoses a popliteal aneurysm, they’ll most likely check your other leg and your belly (abdomen) for aneurysms, too. This is because many people with popliteal aneurysms have another one in their other legs or in their abdomens. If your provider finds any other aneurysms, they’ll likely need to check them with ultrasound throughout your life.
Popliteal aneurysm treatment varies depending on your situation. Your risk of an aneurysm breaking open increases when it gets bigger than 2 centimeters (cm) or almost 1 inch around. This is about twice the normal diameter. If your aneurysm has a blood clot in it, a provider may fix it at a smaller size due to the risk of the clot traveling down your leg and causing a blockage of blood flow.
If your popliteal aneurysm is smaller than 2 cm and you don’t have symptoms, a provider will check it regularly to make sure it’s not growing.
If you have symptoms with your popliteal aneurysm and/or it’s larger than 2 cm (even without symptoms), a provider will do a popliteal aneurysm repair.
In open surgery, a provider treats an aneurysm by tying off the artery above and below it (exclusion) and rerouting the blood flow (bypass). Using a piece of your own vein, they restore blood flow from the artery above the aneurysm to the artery below the aneurysm. Then they tie off (ligate) the aneurysm.
A provider sometimes uses an endovascular approach for people with other chronic conditions or issues that may increase the risk of complications with open surgery. In an endovascular approach, a provider puts a covered stent graft inside your artery across the aneurysm. This diverts blood flow from above the aneurysm to below it. Without direct blood flow, the aneurysm can then clot off around the stent.
Advertisement
If you have a blood clot in your leg and it’s causing lack of blood flow, the treatment is different. In this case, a provider may start by placing you on blood thinners (heparin) through an IV. Then they may attempt to re-establish blood flow to your affected leg and foot by performing an angiogram. In some instances, they can try to dissolve the clot with thrombolytics or remove some of the clot with suction devices.
Complications of popliteal aneurysm treatment may include:
After open surgery, you may be in the hospital for two to three days. Recovery time tends to be shorter for an endovascular approach.
Even if you don’t have popliteal aneurysm symptoms now, you may in the future. Complications are also likely.
A popliteal aneurysm rarely breaks open. You’re more likely to have a blood clot down your leg instead. If you have endovascular surgery, you may have fewer wound complications than with open surgery. But the repair may not last as long.
Your prognosis (outlook) is good if you get a popliteal aneurysm repair before the issue causes symptoms. Researchers found that after five years, the graft was still open to blood flow in 80% of people who received a bypass graft.
Advertisement
If you have symptoms with your aneurysm, your prognosis is worse.
One study found that a little more than half of those who had surgery for a ruptured popliteal aneurysm were alive one year later.
About 15% of people who get a blood clot in their popliteal aneurysm need a leg amputation.
Providers believe atherosclerosis is the main cause of a popliteal aneurysm. You may be able to reduce your risk by:
If you use tobacco products, stopping will improve your health. Also, you can get health benefits from managing these conditions if you have them:
After surgery, you may need to take antiplatelets (aspirin) to decrease the formation of a clot in your bypass. Keep going to all follow-up appointments with your provider. You’ll need routine evaluations of your bypass to make sure it’s staying open. This is important after surgery as well as during the time that your provider is monitoring the popliteal aneurysm to decide on surgery.
Advertisement
After a popliteal aneurysm repair, you’ll need regular ultrasound checks to make sure your artery bypass is staying open. This is important at one, three, six and 12 months after your operation, but also annually for years to come.
Go to the emergency room if you think your popliteal aneurysm has ruptured or embolized. Signs of this include swelling, bruising, pain, numbness, coolness or difficulty moving your affected leg.
You may want to ask your provider:
It can be stressful knowing that you have a popliteal aneurysm. Talk with your provider about when it’s right to fix your aneurysm and what’s best for you. You have the power to improve your health by avoiding tobacco products and managing your blood pressure and cholesterol levels. Ask your provider if you need help.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Vascular disease may affect your life in big and small ways. Cleveland Clinic’s specialists treat the many types of vascular disease so you can focus on living.
